- Record: found
- Abstract: found
- Article: found
Clinical Presentation, Management, and Outcome in Patients With Myasthenia Gravis: A Retrospective Study From Two Tertiary Care Centers in Saudi Arabia
Read this article at
Abstract
Introduction: A limited number of research studies were published to delineate the clinical pattern of myasthenia gravis in Saudi Arabia. This paper is an attempt to describe some of the clinical aspects related to this disease in two large centers from two main cities in Saudi Arabia.
Methods: A retrospective multi-center observational study of patients diagnosed with myasthenia gravis was conducted. The study setting was King Abdulaziz Medical City in Jeddah and Riyadh, Saudi Arabia. The study period was 12 years, starting from January 2007 to May 2019.
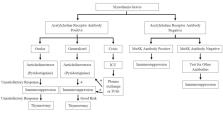
Results: A total of 144 patients were included in this study (60 males and 84 females). The most common symptoms at diagnosis were ocular symptoms in 118 patients (81.9%), diplopia in 84 patients (58.3%), and/or blurred vision in 30 patients (20.8%). The majority had positive anti-acetylcholine receptor antibodies (72.2%). Pyridostigmine was the most prescribed medication for 136 patients (94.4%). Immunosuppressive medications were prescribed for 114 patients (79.2%). Around 40% of patients had exacerbations, and approximately 20% were admitted to the ICU. Thymectomy was performed for 97 patients (67.4%).
Conclusion: The present study indicates that the clinical presentation and management of myasthenia gravis remained the same in the last few years despite the introduction of new modalities of diagnosis such as the anti-muscle-specific kinase (anti-MuSK) and other autoantibodies tests. Furthermore, we observed that the number of exacerbations and ICU admission were high, which may indicate inadequate therapy. We are stressing the need for establishing specialized neuromuscular clinics with neurologists trained in neurophysiology to improve the diagnostic accuracy and outcomes for patients with myasthenia gravis.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Myasthenia gravis
- Record: found
- Abstract: found
- Article: not found
Myasthenia gravis: Association of British Neurologists' management guidelines.
- Record: found
- Abstract: found
- Article: not found