- Record: found
- Abstract: found
- Article: found
National census of UK endoscopy services in 2019
Read this article at
Abstract
Introduction
The 2017 Joint Advisory Group on Gastrointestinal (GI) Endoscopy (JAG) census highlighted the pressure endoscopy services were under in meeting national targets and the factors behind this. In 2019, JAG conducted a further national census of endoscopy services to understand trends in activity, workforce and waiting time targets.
Methods
In April 2019, the census was sent to all eligible JAG-registered services. Collated data were analysed through various statistical methods. A further comparative dataset was created using available submissions from the 2017 census matched to services in the current census.
Results
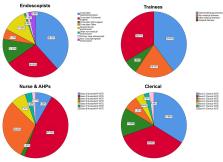
There was a 68% response rate (322/471). There has been a 12%–15% increase in activity across all GI procedures with largest increases in bowel cancer screening. Fewer services are meeting waiting time targets compared with 2017, with endoscopist, nursing and physical capacity cited as the main reasons. Services are striving to improve capacity: 80% of services have an agreed business plan to meet capacity and the number using insourcing has increased from 13% to 20%. The workforce has increased, with endoscopist numbers increasing by 15%, nurses and allied health professionals by 14% and clerical staff by 30%.
Conclusions
The 2019 JAG census is the most recent and extensive survey of UK endoscopy services. There is a clear trend of increasing activity with fewer services able to meet national waiting time targets than 2 years ago. Services have increased their workforce and improved planning to stem the tide but there remains a continued pressure to deliver high quality, safe endoscopy. In light of the COVID-19 pandemic, JAG recognises that these pressures will be severely exacerbated and waiting time targets for accreditation will need adjustment and tolerance during the evolution and recovery from the pandemic.
Related collections
Most cited references19
- Record: found
- Abstract: not found
- Article: not found
Response Rate in Academic Studies-A Comparative Analysis


- Record: found
- Abstract: found
- Article: found