- Record: found
- Abstract: found
- Article: found
Association of Organizational Pathways With the Delay of Emergency Surgery
Read this article at
Abstract
This cohort study examines rates of delayed emergency surgery in French hospitals that have a dedicated emergency surgery department and team, a dedicated emergency operating room, or no dedicated emergency operating room or team.
Key Points
Findings
In this cohort study of 1149 patients, the frequency of delayed emergency surgery was 32.5% and varied substantially across 3 distinct organizational pathways of care: dedicated emergency surgery department and team, dedicated emergency operating room, and no dedicated emergency operating room or team.
Abstract
Importance
Delayed admission of patients with surgical emergencies to the operating room occurs frequently and is associated with poor outcomes. In France, where 3 distinct organizational pathways in hospitals exist (a dedicated emergency operating room and team [DET], a dedicated operating room in a central operating theater [DOR], and no dedicated structure or team [NOR]), neither the incidence nor the influence of delayed urgent surgery is known, and no guidelines are available to date.
Objective
To examine the overall frequency of delayed admission of patients with surgical emergencies to the operating room across the 3 organizational pathways in hospitals in France.
Design, Setting, and Participants
This prospective multicenter cohort study was conducted in 10 French tertiary hospitals. All consecutive adult patients admitted for emergency surgery from October 5 to 16, 2020, were included and prospectively monitored. Patients requiring pediatric surgery, obstetrics, interventional radiology, or endoscopic procedures were excluded.
Main Outcomes and Measures
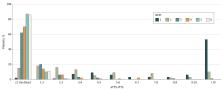
The main outcome was the global incidence of delayed emergency surgery across 3 predefined organizational pathways: DET, DOR, and NOR. The ratio between the actual time to surgery (observed duration between surgical indication and incision) and the ideal time to surgery (predefined optimal duration between surgical indication and incision according to the Non-Elective Surgery Triage classification) was calculated for each patient. Surgery was considered delayed when this ratio was greater than 1.
Results
A total of 1149 patients were included (mean [SD] age, 55 [21] years; 685 [59.9%] males): 649 in the DET group, 320 in the DOR group, and 171 in the NOR group (missing data: n = 5). The global frequency of surgical delay was 32.5% (95% CI, 29.8%-35.3%) and varied across the 3 organizational pathways: DET, 28.4% (95% CI, 24.8%-31.9%); DOR, 32.2% (95% CI, 27.0%-37.4%); and NOR, 49.1% (95% CI, 41.6%-56.7%) ( P < .001). The adjusted odds ratio for delay was 1.80 (95% CI, 1.17-2.78) when comparing NOR with DET.
Conclusions and Relevance
In this cohort study, the frequency of delayed emergency surgery in France was 32.5%. Reduced delays were found in organizational pathways that included dedicated theaters and teams. These preliminary results may pave the way for comprehensive large-scale studies, from which results may potentially inform new guidelines for quicker and safer access to emergency surgery.
Related collections
Most cited references43
- Record: found
- Abstract: not found
- Article: not found
GRADING OF PATIENTS FOR SURGICAL PROCEDURES
- Record: found
- Abstract: found
- Article: not found
Recommended standards for reports dealing with lower extremity ischemia: revised version.
- Record: found
- Abstract: not found
- Article: not found