- Record: found
- Abstract: found
- Article: found
Duration of Adjuvant Doublet Chemotherapy (3 or 6 months) in Patients With High-Risk Stage II Colorectal Cancer
Read this article at
PURPOSE:
As oxaliplatin results in cumulative neurotoxicity, reducing treatment duration without loss of efficacy would benefit patients and healthcare providers.
PATIENTS AND METHODS:
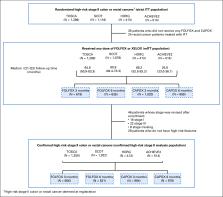
Four of the six studies in the International Duration Evaluation of Adjuvant Chemotherapy (IDEA) collaboration included patients with high-risk stage II colon and rectal cancers. Patients were treated (clinician and/or patient choice) with either fluorouracil, leucovorin, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CAPOX) and randomly assigned to receive 3- or 6-month treatment. The primary end point is disease-free survival (DFS), and noninferiority of 3-month treatment was defined as a hazard ratio (HR) of < 1.2- v 6-month arm. To detect this with 80% power at a one-sided type one error rate of 0.10, a total of 542 DFS events were required.
RESULTS:
3,273 eligible patients were randomly assigned to either 3- or 6-month treatment with 62% receiving CAPOX and 38% FOLFOX. There were 553 DFS events. Five-year DFS was 80.7% and 83.9% for 3-month and 6-month treatment, respectively (HR, 1.17; 80% CI, 1.05 to 1.31; P [for noninferiority] .39). This crossed the noninferiority limit of 1.2. As in the IDEA stage III analysis, the duration effect appeared dependent on the chemotherapy regimen although a test of interaction was negative. HR for CAPOX was 1.02 (80% CI, 0.88 to 1.17), and HR for FOLFOX was 1.41 (80% CI, 1.18 to 1.68).
CONCLUSION:
Although noninferiority has not been demonstrated in the overall population, the convenience, reduced toxicity, and cost of 3-month adjuvant CAPOX suggest it as a potential option for high-risk stage II colon cancer if oxaliplatin-based chemotherapy is suitable. The relative contribution of the factors used to define high-risk stage II disease needs better understanding.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer.
- Record: found
- Abstract: found
- Article: not found
Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer.
- Record: found
- Abstract: found
- Article: not found