- Record: found
- Abstract: found
- Article: found
Thyroid Hormone Supplementation Therapy for Differentiated Thyroid Cancer After Lobectomy: 5 Years of Follow-Up
Read this article at
Abstract
Background: Lobectomy with preservation of the contralateral lobe has already become the most preferred surgical method for patients with low-risk thyroid cancer. The incidence of and risk factors for the development of hypothyroidism after lobectomy for thyroid cancer remains unclear. The previous practice of levothyroxine supplementation post-thyroidectomy, to bring about thyroid stimulating hormone (TSH) suppression, had some serious side effects. This study aimed to evaluate the incidence of hypothyroidism and to identify the factors associated with hypothyroidism requiring thyroid hormone replacement.
Methods: We retrospectively reviewed the charts of 256 consecutive patients with differentiated thyroid cancer treated with lobectomy at the Gangnam Severance Hospital between April and December 2014 who were followed-up for more than 5 years. Patients were evaluated using a thyroid function test at the time of outpatient visit every 6 months for the 1st year, with an annual follow-up thereafter.
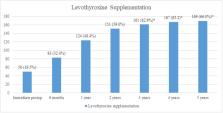
Results: After 5 years, 66.0% (169) of the patients needed levothyroxine supplementation to maintain euthyroid status. The incidence of hypothyroidism requiring levothyroxine supplementation increased until 3 years but showed no significant change in the 4 and 5th year. Recurrence showed no difference between the group with and without levothyroxine supplementation. The presence of thyroiditis and preoperative TSH levels were correlated with postoperative levothyroxine supplementation to maintain euthyroid status, in univariate and multivariate analyses.
Conclusion: High preoperative TSH levels and/or thyroiditis indicate a significantly increased likelihood of developing hypothyroidism requiring thyroid hormone supplementation after a thyroid lobectomy. Patients with an increased risk of postoperative hypothyroidism must be aware of their risk factors and should undergo more intensive follow-ups.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer.
- Record: found
- Abstract: found
- Article: not found
Does postoperative thyrotropin suppression therapy truly decrease recurrence in papillary thyroid carcinoma? A randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found