- Record: found
- Abstract: found
- Article: found
Discovery of key genes as novel biomarkers specifically associated with HPV-negative cervical cancer

Read this article at
Abstract
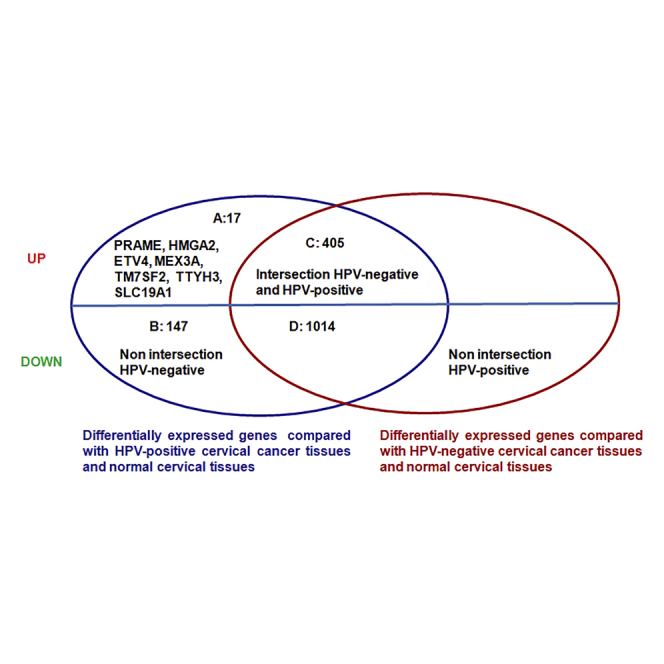
Cervical cancer is a common female malignancy that is mainly caused by human papillomavirus (HPV) infection. However, the incidence of HPV-negative cervical cancer has shown an increasing trend in recent years. Because the mechanism of HPV-negative cervical cancer development is unclear, this study aims to find the pattern of differential gene expression in HPV-negative cervical cancer and verify the underlying potential mechanism. Differentially expressed genes were compared among HPV-positive cervical cancer, HPV-negative cervical cancer, and normal cervical tissues retrieved from TCGA. Subsequently, dysregulated differentially expressed genes specifically existed in HPV-negative cervical cancer tissues and HPV-negative cell lines were validated by qRT-PCR, western blotting, and immunohistochemical staining. We found seventeen highly expressed genes that were particularly associated with HPV-negative cervical cancer from analysis of TCGA database. Among the 17 novel genes, 7 genes (preferentially expressed antigen in melanoma [PRAME], HMGA2, ETS variant 4 [ETV4], MEX3A, TM7SF2, SLC19A1, and tweety-homologs 3 [TTYH3]) displayed significantly elevated expression in HPV-negative cervical cancer cells and HPV-negative cervical cancer tissues. Additionally, higher expression of MEX3A and TTYH3 was associated with a shorter overall survival of patients with HPV-negative cervical cancer. Our study implies that these seven genes are more likely to provide novel insights into the occurrence and progression of HPV-negative cervical cancer.
Graphical abstract
Abstract
The mechanisms of HPV-negative cervical cancer are largely elusive. In this study, the authors discovered the multiple genes in HPV-negative cervical cancer, including PRAME, HMGA2, ETV4, MEX3A, TM7SF2, SLC19A1, and TTYH3, which could contribute to HPV-negative cervical cancer development.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
Cancer Statistics, 2021

- Record: found
- Abstract: found
- Article: found
Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis
- Record: found
- Abstract: found
- Article: not found