- Record: found
- Abstract: found
- Article: found
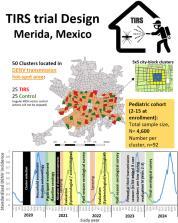
The TIRS trial: protocol for a cluster randomized controlled trial assessing the efficacy of preventive targeted indoor residual spraying to reduce Aedes-borne viral illnesses in Merida, Mexico
Read this article at
Abstract
Background
Current urban vector control strategies have failed to contain dengue epidemics and to prevent the global expansion of Aedes-borne viruses (ABVs: dengue, chikungunya, Zika). Part of the challenge in sustaining effective ABV control emerges from the paucity of evidence regarding the epidemiological impact of any Aedes control method. A strategy for which there is limited epidemiological evidence is targeted indoor residual spraying (TIRS). TIRS is a modification of classic malaria indoor residual spraying that accounts for Aedes aegypti resting behavior by applying residual insecticides on exposed lower sections of walls (< 1.5 m), under furniture, and on dark surfaces.
Methods/design
We are pursuing a two-arm, parallel, unblinded, cluster randomized controlled trial to quantify the overall efficacy of TIRS in reducing the burden of laboratory-confirmed ABV clinical disease (primary endpoint). The trial will be conducted in the city of Merida, Yucatan State, Mexico (population ~ 1million), where we will prospectively follow 4600 children aged 2–15 years at enrollment, distributed in 50 clusters of 5 × 5 city blocks each. Clusters will be randomly allocated ( n = 25 per arm) using covariate-constrained randomization. A “fried egg” design will be followed, in which all blocks of the 5 × 5 cluster receive the intervention, but all sampling to evaluate the epidemiological and entomological endpoints will occur in the “yolk,” the center 3 × 3 city blocks of each cluster. TIRS will be implemented as a preventive application (~ 1–2 months prior to the beginning of the ABV season). Active monitoring for symptomatic ABV illness will occur through weekly household visits and enhanced surveillance. Annual sero-surveys will be performed after each transmission season and entomological evaluations of Ae. aegypti indoor abundance and ABV infection rates monthly during the period of active surveillance. Epidemiological and entomological evaluation will continue for up to three transmission seasons.
Discussion
The findings from this study will provide robust epidemiological evidence of the efficacy of TIRS in reducing ABV illness and infection. If efficacious, TIRS could drive a paradigm shift in Aedes control by considering Ae. aegypti behavior to guide residual insecticide applications and changing deployment to preemptive control (rather than in response to symptomatic cases), two major enhancements to existing practice.
Trial registration
ClinicalTrials.gov NCT04343521. Registered on 13 April 2020. The protocol also complies with the WHO International Clinical Trials Registry Platform (ICTRP) (Additional file 1).
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
Dengue, Urbanization and Globalization: The Unholy Trinity of the 21st Century

- Record: found
- Abstract: found
- Article: found
Contemporary status of insecticide resistance in the major Aedes vectors of arboviruses infecting humans
- Record: found
- Abstract: found
- Article: not found