- Record: found
- Abstract: found
- Article: found
Learning Curve for a Laparoscopic Appendectomy by a Surgical Trainee

Read this article at
Abstract
Purpose
The laparoscopic appendectomy has been a basic part of the principal of a more complex laparoscopic technique for the surgical trainee. As the number of laparoscopic appendectomies performed by surgical trainees has increased, we are trying to check the stability of, which is controversial, and the learning curve associated with a laparoscopic appendectomy.
Methods
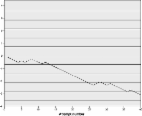
We studied the demographics, histologic diagnoses, operative time, the number of complicated cases, and hospital duration of one hundred and three patients who underwent an open appendectomy (group A, 53) or a laparoscopic appendectomy (group B, 50) retrospectively through a review of their medical records. The learning curve for the laparoscopic appendectomy was established through the moving average and ANOVA methods.
Results
There were no differences in the operative times (A, 64.15 ± 29.88 minutes; B, 58.2 ± 20.72 minutes; P-value, 0.225) and complications (A, 11%; B, 6%; P-value, 0.34) between group A and group B. Group B was divided into group C who underwent the operation in the early period (before the learning curve) and group D who underwent the operation in the later period (after the learning curve). The average operative time for group C was 66.83 ± 21.55 minutes, but it was 45.25 ± 10.19 minutes for group D (P-value < 0.0001). Although this difference was statistically significant, no significant difference in the complication rate was observed between the two groups.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Laparoscopic appendectomy by residents: evaluating outcomes and learning curve.
- Record: found
- Abstract: found
- Article: found
Laparoscopic Appendectomy: a Junior Trainee's Learning Curve
- Record: found
- Abstract: found
- Article: not found