- Record: found
- Abstract: found
- Article: found
Interplay between diabetes mellitus and periodontal/pulpal-periapical diseases
Read this article at
Abstract
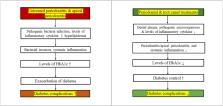
This longevity of life expectancy has indirectly led to an increase in the number of chronic diseases such as periodontitis, apical periodontitis (AP), and diabetes mellitus (DM) in the aging society, thus affecting people's quality of life. There is an interaction between periodontitis/AP and DM with a two-way relationship. Although type 1 and 2 diabetes (T1DM, T2DM) have different etiologies, glycemic control may affect the infection, inflammation and tissue healing of periodontitis and AP. Non-surgical periodontal treatment may influence the glycemic control as shown by decrease of HbA1c level in T2DM patient. However, the effect of periodontal treatment on glycemic control in T1DM and root canal treatment/apical surgery on T1DM and T2DM patients awaits investigation. DM may affect the periodontal and periapical tissues possibly via altered oral microbiota, impairment of neutrophils' activity and host immune responses and cytokine production, induction of oxidative stress etc. While periodontitis associated systemic inflammation and hyperlipidemia is suggested to contribute to the control of T2DM, more intricate studies are necessary to clarify the detailed mechanisms. The interactions between DM (T1DM and T2DM) and periodontitis and AP are therefore reviewed to provide a basis for the treatment of subsequent patients with pulpal/periodontal disease and diabetes. A two-pronged approach of medical and dental treatment is needed for the management of these patients, with emphasis on blood glucose control and improving oral hygiene and periodontal maintenance care, to ensure the best treatment outcome.
Related collections
Most cited references92
- Record: found
- Abstract: found
- Article: not found
Global estimates of the prevalence of diabetes for 2010 and 2030.
- Record: found
- Abstract: found
- Article: not found