- Record: found
- Abstract: found
- Article: found
A shortened verbal autopsy instrument for use in routine mortality surveillance systems

Read this article at
Abstract
Background
Verbal autopsy (VA) is recognized as the only feasible alternative to comprehensive medical certification of deaths in settings with no or unreliable vital registration systems. However, a barrier to its use by national registration systems has been the amount of time and cost needed for data collection. Therefore, a short VA instrument (VAI) is needed. In this paper we describe a shortened version of the VAI developed for the Population Health Metrics Research Consortium (PHMRC) Gold Standard Verbal Autopsy Validation Study using a systematic approach.
Methods
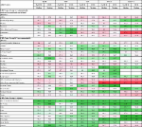
We used data from the PHMRC validation study. Using the Tariff 2.0 method, we first established a rank order of individual questions in the PHMRC VAI according to their importance in predicting causes of death. Second, we reduced the size of the instrument by dropping questions in reverse order of their importance. We assessed the predictive performance of the instrument as questions were removed at the individual level by calculating chance-corrected concordance and at the population level with cause-specific mortality fraction (CSMF) accuracy. Finally, the optimum size of the shortened instrument was determined using a first derivative analysis of the decline in performance as the size of the VA instrument decreased for adults, children, and neonates.
Results
The full PHMRC VAI had 183, 127, and 149 questions for adult, child, and neonatal deaths, respectively. The shortened instrument developed had 109, 69, and 67 questions, respectively, representing a decrease in the total number of questions of 40-55 %. The shortened instrument, with text, showed non-significant declines in CSMF accuracy from the full instrument with text of 0.4 %, 0.0 %, and 0.6 % for the adult, child, and neonatal modules, respectively.
Conclusions
We developed a shortened VAI using a systematic approach, and assessed its performance when administered using hand-held electronic tablets and analyzed using Tariff 2.0. The length of a VA questionnaire was shortened by almost 50 % without a significant drop in performance. The shortened VAI developed reduces the burden of time and resources required for data collection and analysis of cause of death data in civil registration systems.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Civil registration systems and vital statistics: successes and missed opportunities.

- Record: found
- Abstract: found
- Article: found
Population Health Metrics Research Consortium gold standard verbal autopsy validation study: design, implementation, and development of analysis datasets
- Record: found
- Abstract: found
- Article: found