- Record: found
- Abstract: found
- Article: found
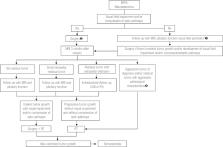
A review on the diagnosis and treatment of patients with clinically nonfunctioning pituitary adenoma by the Neuroendocrinology Department of the Brazilian Society of Endocrinology and Metabolism
ABSTRACT
Clinically nonfunctioning pituitary adenomas (NFPA) are the most common pituitary tumors after prolactinomas. The absence of clinical symptoms of hormonal hypersecretion can contribute to the late diagnosis of the disease. Thus, the majority of patients seek medical attention for signs and symptoms resulting from mass effect, such as neuro-ophthalmologic symptoms and hypopituitarism. Other presentations include pituitary apoplexy or an incidental finding on imaging studies. Mass effect and hypopituitarism impose high morbidity and mortality. However, early diagnosis and effective treatment minimizes morbidity and mortality. In this publication, the goal of the Neuroendocrinology Department of the Brazilian Society of Endocrinology and Metabolism is to provide a review of the diagnosis and treatment of patients with NFPA, emphasizing that the treatment should be performed in reference centers. This review is based on data published in the literature and the authors’ experience. Arch Endocrinol Metab. 2016;60(4):374-90
Related collections
Most cited references250
- Record: found
- Abstract: found
- Article: not found
The prevalence of pituitary adenomas: a systematic review.
- Record: found
- Abstract: found
- Article: not found
The diagnosis of Cushing's syndrome: an Endocrine Society Clinical Practice Guideline.
- Record: found
- Abstract: found
- Article: not found