- Record: found
- Abstract: found
- Article: not found
Risk of hydroxychloroquine alone and in combination with azithromycin in the treatment of rheumatoid arthritis: a multinational, retrospective study
Read this article at
- open (via crossref license)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH doi match)
- oa repository (via OAI-PMH title and first author match)
- oa repository (via pmcid lookup)
- oa repository (via page says license)
Powered by 
Summary
Background
Hydroxychloroquine, a drug commonly used in the treatment of rheumatoid arthritis, has received much negative publicity for adverse events associated with its authorisation for emergency use to treat patients with COVID-19 pneumonia. We studied the safety of hydroxychloroquine, alone and in combination with azithromycin, to determine the risk associated with its use in routine care in patients with rheumatoid arthritis.
Methods
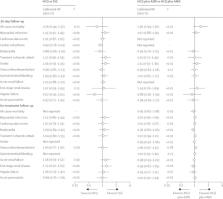
In this multinational, retrospective study, new user cohort studies in patients with rheumatoid arthritis aged 18 years or older and initiating hydroxychloroquine were compared with those initiating sulfasalazine and followed up over 30 days, with 16 severe adverse events studied. Self-controlled case series were done to further establish safety in wider populations, and included all users of hydroxychloroquine regardless of rheumatoid arthritis status or indication. Separately, severe adverse events associated with hydroxychloroquine plus azithromycin (compared with hydroxychloroquine plus amoxicillin) were studied. Data comprised 14 sources of claims data or electronic medical records from Germany, Japan, the Netherlands, Spain, the UK, and the USA. Propensity score stratification and calibration using negative control outcomes were used to address confounding. Cox models were fitted to estimate calibrated hazard ratios (HRs) according to drug use. Estimates were pooled where the I 2 value was less than 0·4.
Findings
The study included 956 374 users of hydroxychloroquine, 310 350 users of sulfasalazine, 323 122 users of hydroxychloroquine plus azithromycin, and 351 956 users of hydroxychloroquine plus amoxicillin. No excess risk of severe adverse events was identified when 30-day hydroxychloroquine and sulfasalazine use were compared. Self-controlled case series confirmed these findings. However, long-term use of hydroxychloroquine appeared to be associated with increased cardiovascular mortality (calibrated HR 1·65 [95% CI 1·12–2·44]). Addition of azithromycin appeared to be associated with an increased risk of 30-day cardiovascular mortality (calibrated HR 2·19 [95% CI 1·22–3·95]), chest pain or angina (1·15 [1·05–1·26]), and heart failure (1·22 [1·02–1·45]).
Interpretation
Hydroxychloroquine treatment appears to have no increased risk in the short term among patients with rheumatoid arthritis, but in the long term it appears to be associated with excess cardiovascular mortality. The addition of azithromycin increases the risk of heart failure and cardiovascular mortality even in the short term. We call for careful consideration of the benefit–risk trade-off when counselling those on hydroxychloroquine treatment.
Funding
National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, NIHR Senior Research Fellowship programme, US National Institutes of Health, US Department of Veterans Affairs, Janssen Research and Development, IQVIA, Korea Health Industry Development Institute through the Ministry of Health and Welfare Republic of Korea, Versus Arthritis, UK Medical Research Council Doctoral Training Partnership, Foundation Alfonso Martin Escudero, Innovation Fund Denmark, Novo Nordisk Foundation, Singapore Ministry of Health's National Medical Research Council Open Fund Large Collaborative Grant, VINCI, Innovative Medicines Initiative 2 Joint Undertaking, EU's Horizon 2020 research and innovation programme, and European Federation of Pharmaceutical Industries and Associations.
Related collections
Most cited references25

- Record: found
- Abstract: found
- Article: found
Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro
- Record: found
- Abstract: found
- Article: not found
Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial
- Record: found
- Abstract: found
- Article: not found