- Record: found
- Abstract: found
- Article: found
Acoustic Micro-Tapping Optical Coherence Elastography to Quantify Corneal Collagen Cross-Linking : An Ex Vivo Human Study
Read this article at
Abstract
Purpose
To evaluate changes in the anisotropic elastic properties of ex vivo human cornea treated with ultraviolet cross-linking (CXL) using noncontact acoustic micro-tapping optical coherence elastography (AμT-OCE).
Design
Acoustic micro-tapping OCE was performed on normal and CXL human donor cornea in an ex vivo laboratory study.
Subjects
Normal human donor cornea (n = 22) divided into 4 subgroups. All samples were stored in optisol.
Methods
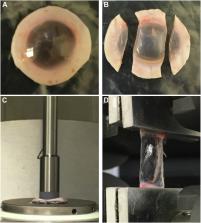
Elastic properties (in-plane Young’s, E, and out-of-plane, G, shear modulus) of normal and ultraviolet CXL–treated human corneas were quantified using noncontact AμT-OCE. A nearly incompressible transverse isotropic model was used to reconstruct moduli from AμT-OCE data. Independently, cornea elastic moduli were also measured with destructive mechanical tests (tensile extensometry and shear rheometry).
Main Outcome Measures
Corneal elastic moduli (in-plane Young’s modulus, E, in-plane, μ, and out-of-plane, G, shear moduli) can be evaluated in both normal and CXL treated tissues, as well as monitored during the CXL procedure using noncontact AμT-OCE.
Results
Cross-linking induced a significant increase in both in-plane and out-of-plane elastic moduli in human cornea. The statistical mean in the paired study (presurgery and postsurgery, n = 7) of the in-plane Young’s modulus, , increased from 19 MPa to 43 MPa, while the out-of-plane shear modulus, G, increased from 188 kPa to 673 kPa. Mechanical tests in a separate subgroup support CXL-induced cornea moduli changes and generally agree with noncontact AμT-OCE measurements.
Related collections
Most cited references76
- Record: found
- Abstract: found
- Article: not found
Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking.
- Record: found
- Abstract: found
- Article: not found
Safety of UVA-riboflavin cross-linking of the cornea.
- Record: found
- Abstract: found
- Article: not found