- Record: found
- Abstract: found
- Article: found
Seroprevalence of anti-SARS-CoV-2 IgG among healthcare workers of a large university hospital in Milan, Lombardy, Italy: a cross-sectional study
Read this article at
Abstract
Objectives
To assess the seroprevalence of anti-SARS-CoV-2 IgG among health careworkers (HCWs) in our university hospital and verify the risk of acquiring the infection according to work area.
Participants
All the employees of the hospital on a voluntary base, for a total of 4055 participants among 4572 HCWs (88.7%).
Primary and secondary outcome measures
Number of anti-SARS-CoV-2 positive serology according to working area. Association of anti-SARS-CoV-2 positive serology to selected variables (age, gender, country of origin, body mass index, smoking, symptoms and contact with confirmed cases).
Results
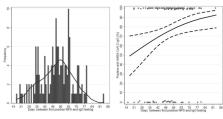
From 27 April 2020 to 12 June 2020, 4055 HCWs were tested and 309 (7.6%) had a serological positive test. No relevant difference was found between men and women (8.3% vs 7.3%, p=0.3), whereas a higher prevalence was observed among foreign-born workers (27/186, 14.5%, p<0.001), employees younger than 30 (64/668, 9.6%, p=0.02) or older than 60 years (38/383, 9.9%, p=0.02) and among healthcare assistants (40/320, 12.5%, p=0.06). Working as frontline HCWs was not associated with an increased frequency of positive serology (p=0.42). A positive association was found with presence and number of symptoms (p<0.001). The symptoms most frequently associated with a positive serology were taste and smell alterations (OR 4.62, 95% CI: 2.99 to 7.15) and fever (OR 4.37, 95% CI: 3.11 to 6.13). No symptoms were reported in 84/309 (27.2%) HCWs with positive IgG levels. Declared exposure to a suspected/confirmed case was more frequently associated (p<0.001) with positive serology when the contact was a family member (19/94, 20.2%) than a patient or colleague (78/888, 8.8%).
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans

- Record: found
- Abstract: found
- Article: found