- Record: found
- Abstract: found
- Article: found
Short-term results of laparoscopic anti-reflux surgery with the RefluxStop device in patients with gastro-esophageal reflux disease and ineffective esophageal motility
Read this article at
Abstract
Purpose
In gastro-esophageal reflux disease (GERD) requiring surgical treatment, concomitant ineffective esophageal motility (IEM) is a decisive factor in surgical planning, due to concern regarding dysphagia. Anti-reflux surgery with the RefluxStop device is a promising technique. We assessed initial feasibility and clinical outcomes of RefluxStop surgery in patients with GERD and IEM.
Methods
Retrospective analysis of patients with GERD, hiatal hernia (HH), and IEM, who underwent surgery with RefluxStop at our institution and achieved 12-month follow-up. Technique feasibility was assessed, in addition to symptom resolution (GERD-HRQL questionnaire), adverse events, HH recurrence, dysphagia, and patient satisfaction. Placement of the device was confirmed by video fluoroscopy on postoperative day 1, and at 3 and 12 months.
Results
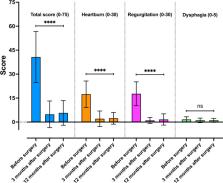
Between June 2020 and November 2022, 20 patients with IEM underwent surgery with RefluxStop and completed 12-month follow-up. All patients reported typical symptoms of GERD, and 12 had preoperative dysphagia. The median HH length was 4.5 cm (IQR, 3.75–5). The median operating time was 59.5 min (IQR, 50.25–64) with no implant-related intra- or postoperative complications. No HH recurrence was observed. One patient reported persistent left-sided thoracic pain at 11 months post-surgery, which required diagnostic laparoscopy and adhesiolysis. Three patients reported severe postoperative dysphagia: balloon dilatation was performed towards resolution. The mean GERD-HRQL scores improved (from 40.7 at baseline to 4.8 at 3 months and 5.7 at 12 months ( p <0.001)).
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey.
- Record: found
- Abstract: found
- Article: not found
Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification.
- Record: found
- Abstract: found
- Article: not found