- Record: found
- Abstract: found
- Article: found
A systematic review of risk factors and adverse outcomes associated with anterior cervical discectomy and fusion surgery over the past decade
Read this article at
ABSTRACT
Background:
Anterior cervical discectomy and fusion (ACDF) is one of the most frequently performed cervical surgeries in the world, yet there have been several reported complications.
Objective:
To determine the actual incidence of complications related to ACDF as well as any risk variables that may have been identified in earlier research.
Methods:
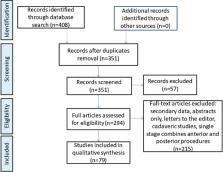
To evaluate the origin, presentation, natural history, and management of the risks and the complications, we conducted a thorough assessment of the pertinent literature. An evaluation of clinical trials and case studies of patients who experienced one or more complications following ACDF surgery was done using a PubMed, Cochrane Library, and Google Scholar search. Studies involving adult human subjects that were written in the English language and published between 2012 and 2022 were included in the search. The search yielded 79 studies meeting our criteria.
Results:
The overall rates of complications were as follows: Dysphagia 7.9%, psudarthrosis 5.8%, adjacent segment disease (ASD) 8.8%, esophageal perforations (EPs) 0.5%, graft or hardware failure 2.2%, infection 0.3%, recurrent laryngeal nerve palsy 1.7%, cerebrospinal fluid leak 0.8%, Horner syndrome 0.5%, hematoma 0.8%, and C5 palsy 1.9%.
Conclusion:
Results showed that dysphagia was a common postoperative sequelae with bone morphogenetic protein use and a higher number of surgical levels being the major risk factors. Pseudarthrosis rates varied depending on the factors such as asymptomatic radiographic graft sinking, neck pain, or radiculopathy necessitating revision surgery. The incidence of ASD indicated no data to support anterior cervical plating as more effective than standalone ACDF. EP was rare but frequently fatal, with no correlation found between patient age, sex, body mass index, operation time, or number of levels.
Related collections
Most cited references83
- Record: found
- Abstract: not found
- Article: not found
The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion.
- Record: found
- Abstract: found
- Article: not found
Anterior cervical spine surgery-associated complications in a retrospective case-control study
- Record: found
- Abstract: found
- Article: not found