- Record: found
- Abstract: found
- Article: found
Gauging the impact of the COVID-19 pandemic on tuberculosis services: a global study
Abstract
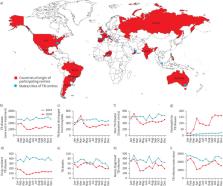
The effects of the coronavirus disease 2019 (COVID-19) pandemic on tuberculosis (TB) disease and TB services emerged in the beginning of 2020 [1, 2]. Epidemiological and clinical studies, including mortality rates of the first cohort of patients with COVID-19 and TB co-infection were described [3, 4]. Several reports from individual countries suggested that the COVID-19 pandemic significantly affected TB services [5–9], including validation by modelling studies [10]. The Global Tuberculosis Network (GTN) reported that the COVID-19 pandemic affected TB services in 33 TB centres from 16 countries in the first 4 months of 2020 [11]. An increased use of telehealth during the COVID-19 pandemic was observed in some TB centres [11]. The major limitations of that study were the short period of observation (January to April 2020 compared to the same period in 2019) and the limited number of variables analysed [11–14].
Abstract
This global study of 43 TB centres from 19 countries demonstrates the impact of COVID-19 pandemic on TB services. Newly diagnosed TB disease, drug-resistant TB, TB deaths, outpatient clinic attendances and newly diagnosed TB infection were reduced. https://bit.ly/3sdHbfk
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: found
Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases
- Record: found
- Abstract: found
- Article: not found
The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis
- Record: found
- Abstract: found
- Article: not found