- Record: found
- Abstract: found
- Article: found
Characteristics and outcomes of culture-negative versus culture-positive severe sepsis
Read this article at
Abstract
Introduction
Culture-negative sepsis is a common but relatively understudied condition. The aim of this study was to compare the characteristics and outcomes of culture-negative versus culture-positive severe sepsis.
Methods
This was a prospective observational cohort study of 1001 patients who were admitted to the medical intensive care unit (ICU) of a university hospital from 2004 to 2009 with severe sepsis. Patients with documented fungal, viral, and parasitic infections were excluded.
Results
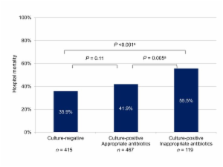
There were 415 culture-negative patients (41.5%) and 586 culture-positive patients (58.5%). Gram-positive bacteria were isolated in 257 patients, and gram-negative bacteria in 390 patients. Culture-negative patients were more often women and had fewer comorbidities, less tachycardia, higher blood pressure, lower procalcitonin levels, lower Acute Physiology and Chronic Health Evaluation II (median 25.0 (interquartile range 19.0 to 32.0) versus 27.0 (21.0 to 33.0), P = 0.001) and Sequential Organ Failure Assessment scores, less cardiovascular, central nervous system, and coagulation failures, and less need for vasoactive agents than culture-positive patients. The lungs were a more common site of infection, while urinary tract, soft tissue and skin infections, infective endocarditis and primary bacteremia were less common in culture-negative than in culture-positive patients. Culture-negative patients had a shorter duration of hospital stay (12 days (7.0 to 21.0) versus 15.0 (7.0 to27.0), P = 0.02) and lower ICU mortality than culture-positive patients. Hospital mortality was lower in the culture-negative group (35.9%) than in the culture-positive group (44.0%, P = 0.01), the culture-positive subgroup, which received early appropriate antibiotics (41.9%, P = 0.11), and the culture-positive subgroup, which did not (55.5%, P < 0.001). After adjusting for covariates, culture positivity was not independently associated with mortality on multivariable analysis.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
The international sepsis forum consensus conference on definitions of infection in the intensive care unit.
- Record: found
- Abstract: found
- Article: not found