- Record: found
- Abstract: found
- Article: found
Peer-assisted learning after onsite, low-dose, high-frequency training and practice on simulators to prevent and treat postpartum hemorrhage and neonatal asphyxia: A pragmatic trial in 12 districts in Uganda
Read this article at
Abstract
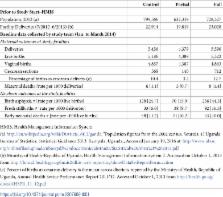
An urgent need exists to improve and maintain intrapartum skills of providers in sub-Saharan Africa. Peer-assisted learning may address this need, but few rigorous evaluations have been conducted in real-world settings. A pragmatic, cluster-randomized trial in 12 Ugandan districts provided facility-based, team training for prevention and management of postpartum hemorrhage and birth asphyxia at 125 facilities. Three approaches to facilitating simulation-based, peer assisted learning were compared. The primary outcome was the proportion of births with uterotonic given within one minute of birth. Outcomes were evaluated using observation of birth and supplemented by skills assessments and service delivery data. Individual and composite variables were compared across groups, using generalized linear models. Overall, 107, 195, and 199 providers were observed at three time points during 1,716 births across 44 facilities. Uterotonic coverage within one minute increased from: full group: 8% (CI 4%‒12%) to 50% (CI 42%‒59%); partial group: 19% (CI 9%‒30%) to 42% (CI 31%‒53%); and control group: 11% (5%‒7%) to 51% (40%‒61%). Observed care of mother and newborn improved in all groups. Simulated skills maintenance for postpartum hemorrhage prophylaxis remained high across groups 7 to 8 months after the intervention. Simulated skills for newborn bag-and-mask ventilation remained high only in the full group. For all groups combined, incidence of postpartum hemorrhage and retained placenta declined 17% and 47%, respectively, from during the intervention period compared to the 6‒9 month period after the intervention. Fresh stillbirths and newborn deaths before discharge decreased by 34% and 62%, respectively, from baseline to after completion, and remained reduced 6‒9 months post-implementation. Significant improvements in uterotonic coverage remained across groups 6 months after the intervention. Findings suggest that while short, simulation-based training at the facility improves care and is feasible, more complex clinical skills used infrequently such as newborn resuscitation may require more practice to maintain skills.
Trial Registration: ClinicalTrials.gov NCT03254628.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: found
Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013
- Record: found
- Abstract: found
- Article: not found
Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training.
- Record: found
- Abstract: found
- Article: not found