- Record: found
- Abstract: found
- Article: found
Dairy Intake and Acne Vulgaris: A Systematic Review and Meta-Analysis of 78,529 Children, Adolescents, and Young Adults
Read this article at
Abstract
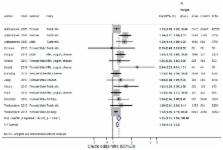
A meta-analysis can help inform the debate about the epidemiological evidence on dairy intake and development of acne. A systematic literature search of PubMed from inception to 11 December 2017 was performed to estimate the association of dairy intake and acne in children, adolescents, and young adults in observational studies. We estimated the pooled random effects odds ratio (OR) (95% CI), heterogeneity ( I 2-statistics, Q-statistics), and publication bias. We included 14 studies ( n = 78,529; 23,046 acne-cases/55,483 controls) aged 7–30 years. ORs for acne were 1.25 (95% CI: 1.15–1.36; p = 6.13 × 10 −8) for any dairy, 1.22 (1.08–1.38; p = 1.62 × 10 −3) for full-fat dairy, 1.28 (1.13–1.44; p = 8.23 × 10 −5) for any milk, 1.22 (1.06–1.41; p = 6.66 × 10 −3) for whole milk, 1.32 (1.16–1.52; p = 4.33 × 10 −5) for low-fat/skim milk, 1.22 (1.00–1.50; p = 5.21 × 10 −2) for cheese, and 1.36 (1.05–1.77; p = 2.21 × 10 −2) for yogurt compared to no intake. ORs per frequency of any milk intake were 1.24 (0.95–1.62) by 2–6 glasses per week, 1.41 (1.05–1.90) by 1 glass per day, and 1.43 (1.09–1.88) by ≥2 glasses per day compared to intake less than weekly. Adjusted results were attenuated and compared unadjusted. There was publication bias ( p = 4.71 × 10 −3), and heterogeneity in the meta-analyses were explained by dairy and study characteristics. In conclusion, any dairy, such as milk, yogurt, and cheese, was associated with an increased OR for acne in individuals aged 7–30 years. However, results should be interpreted with caution due to heterogeneity and bias across studies.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Acne vulgaris.
- Record: found
- Abstract: found
- Article: not found