- Record: found
- Abstract: found
- Article: found
Trends in Outbreak-Associated Cases of COVID-19 — Wisconsin, March–November 2020
research-article

Ian W. Pray , PhD
1
,
2
,
3
,
,
Anna Kocharian , MS
1 ,
Jordan Mason , DVM
1 ,
Ryan Westergaard , MD
1
,
4 ,
Jonathan Meiman , MD
1
29 January 2021
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
During September 3–November 16, 2020, daily confirmed cases of coronavirus disease
2019 (COVID-19) reported to the Wisconsin Department of Health Services (WDHS) increased
at a rate of 24% per week, from a 7-day average of 674 (August 28–September 3) to
6,426 (November 10–16) (
1
). The growth rate during this interval was the highest to date in Wisconsin and among
the highest in the United States during that time (
1
). To characterize potential sources of this increase, the investigation examined
reported outbreaks in Wisconsin that occurred during March 4–November 16, 2020, with
respect to their setting and number of associated COVID-19 cases.
Outbreaks were defined as the occurrence of two or more confirmed COVID-19 cases*
among persons who worked or lived together or among persons who attended the same
facility or event, did not share a household, and were identified within 14 days of
each other (by symptom onset date or sample collection date). During March 4–November
16, local and tribal health departments in Wisconsin reported suspected COVID-19 outbreaks
to WDHS using established reporting criteria
†
; 5,757 reported outbreaks meeting the outbreak definition were included in the analysis.
Confirmed cases of COVID-19 that were linked
§
to these outbreaks were analyzed by symptom onset date (or sample collection date),
the reported setting
¶
of the associated outbreak or outbreaks during three periods: before and during Wisconsin’s
Safer At Home order** (March 4–May 12), summer and return-to-school (May 13–September
2), and the exponential growth phase
††
(September 3–November 16). This activity was reviewed by CDC and was conducted in
a manner consistent with applicable federal law and CDC policy.
§§
A total of 57,991 confirmed cases of COVID-19 were linked to 5,757 outbreaks during
March 4–November 16, accounting for 18.3% of 316,758 confirmed cases in Wisconsin
during this period (Table). Overall, outbreaks at long-term care facilities (26.8%),
correctional facilities (14.9%), and colleges or universities (15.0%) accounted for
the largest numbers of outbreak-associated cases in Wisconsin. Before and during Wisconsin’s
Safer At Home order, 4,552 outbreak-associated cases were linked to 507 reported outbreaks.
Outbreaks at manufacturing or food processing facilities (2,146 cases; 47.1%) and
long-term care facilities (1,324 cases; 29.1%) accounted for the majority of outbreak-associated
cases during this period (Figure). During May 13–September 2, a total of 13,506 cases
were linked to 2,444 outbreaks. Long-term care facilities (2,850 cases; 21.1%) and
manufacturing or food processing facilities (2,672 cases; 19.8%) continued to account
for the largest number of outbreak-associated cases during this period. However, a
variety of other settings including restaurants and bars (1,633 cases; 12.1%) and
other workplaces (1,320 cases; 9.8%) accounted for an increasing proportion of outbreak-associated
cases until mid-August, when a sharp increase in college- and university-associated
outbreaks was observed (1,739 cases; 12.9%). Beginning on September 3, COVID-19 cases
in Wisconsin increased exponentially overall and within outbreak settings. During
this phase of increasing community transmission, 39,933 cases were associated with
3,861 reported outbreaks, which accounted for 16.7% of 239,629 confirmed cases in
Wisconsin. Among outbreak-associated cases, 11,386 (28.5%) were associated with long-term
care facilities, 7,397 (18.5%) with correctional facilities, 7,178 (18.0%) with colleges
or universities, and 5,703 (14.3%) with schools or child care facilities. During this
period of exponential growth, the number of cases associated with long-term care and
correctional facilities increased by an average of 24% and 23% per week, respectively.
TABLE
Laboratory-confirmed COVID-19 cases associated with outbreaks by settings, and period
of the COVID-19 response — Wisconsin, March–November 2020
Outbreak setting
No. (%)
Mar 4–May 12
May 13–Sep 2
Sep 3–Nov 16
Total
Long-term care facility
1,324 (29.1)
2,850 (21.1)
11,386 (28.5)
15,529 (26.8)
College or university
36 (0.8)
1,739 (12.9)
7,178 (18.0)
8,689 (15.0)
Correctional facility
307 (6.7)
964 (7.1)
7,397 (18.5)
8,661 (14.9)
K–12 school or child care facility
10 (0.2)
461 (3.4)
5,704 (14.3)
6,145 (10.6)
Food production or manufacturing facility*
2,146 (47.1)
2,672 (19.8)
3,631 (9.1)
8,436 (14.5)
Restaurant or bar
82 (1.8)
1,633 (12.1)
917 (2.3)
2,628 (4.5)
Retail or public establishment
45 (1.0)
814 (6.0)
1,053 (2.6)
1,902 (3.3)
Event or gathering
39 (0.9)
761 (5.6)
1,113 (2.8)
1,885 (3.3)
Health care facility
115 (2.5)
444 (3.3)
1,214 (3.0)
1,768 (3.0)
Other group housing facility
249 (5.5)
352 (2.6)
781 (2.0)
1,375 (2.4)
Other workplaces†
292 (6.4)
1,320 (9.8)
1,985 (5.0)
3,585 (6.2)
Other settings
48 (1.1)
794 (5.9)
1,424 (3.6)
2,222 (3.8)
Total§
4,552
13,506
39,933
57,991
Abbreviations: COVID-19 = coronavirus disease 2019; K–12 = kindergarten through grade
12.
* Includes food production and processing, meat processing, manufacturing facilities,
and distribution or warehouse facilities.
† Includes agriculture, farming, forestry, construction, contracting, office or other
indoor workplace, public safety, transportation, and utilities.
§ Some cases were associated with multiple outbreak settings because multiple epidemiologic
linkages were identified during the outbreak investigation; thus, the sum of all categories
exceeds the total number of cases listed for each period.
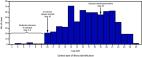
FIGURE
Trends* in the number of laboratory-confirmed COVID-19 cases associated with outbreaks,
by setting
†
and period of the COVID-19 response — Wisconsin, March–November 2020
Abbreviations: COVID-19 = coronavirus disease 2019; K–12 = kindergarten through grade
12.
* Data from November 10–16, 2020 are not displayed in the figure, but are represented
in the counts that appear in text and footnotes.
† All other categories includes restaurant or bar (4.2%), retail or other public establishment
(3.1%), event or gathering (3.0%), health care facility (2.8%), other group housing
(2.2%), other workplaces (5.7%), and other settings (3.5%).
The figure is a line chart showing trends in the number of laboratory-confirmed COVID-19
cases associated with outbreaks, by setting and period, in Wisconsin during March–November
2020.
Discussion
The majority of outbreak-associated COVID-19 cases in Wisconsin occurred in long-term
care facilities, correctional facilities, and colleges and universities; however,
various settings were affected by COVID-19 outbreaks over the course of March–November
2020. During Wisconsin’s Safer At Home order, outbreaks were concentrated in manufacturing
and food processing facilities, which continued to operate as essential businesses
under the statewide order. This aligned with national data showing a high incidence
of COVID-19 outbreaks at meat processing facilities across the United States during
this time, including among beef and pork processing facilities in Wisconsin (
2
). During early summer (June–July), outbreaks continued to occur in long-term care
facilities and manufacturing and food processing facilities; restaurants and bars,
other workplaces, events, and other public establishments were increasingly reported
as outbreak settings, which might have corresponded to fewer restrictions on social
gatherings and decreased risk perception among some groups during this period (
3
).
In late August, a rapid increase in cases associated with outbreaks at colleges and
universities in Wisconsin occurred, correlating with return to campus for many of
these institutions. This pattern was consistent with national trends for COVID-19
among young adults aged 18–22 years (
4
) and corresponded with outbreaks observed at colleges and universities in other states
during this time (
5
). In Wisconsin, the college and university surge occurred at the beginning of a period
of increasing community transmission, which was characterized by exponential growth
in COVID-19 incidence across the state and a surge of outbreaks in high-risk congregate
settings such as long-term care facilities and correctional facilities. The extent
to which COVID-19 outbreaks on college and university campuses led to increased community
transmission and subsequent outbreaks in other high-risk congregate settings could
not be directly assessed in this investigation. Nonetheless, the temporal correlation
observed builds on prior evidence of increased incidence of COVID-19 among U.S. counties
where in-person university instruction occurred in August 2020 (
6
), suggesting that outbreaks on college and university campuses could represent early
indicators of community transmission and should be prioritized for surveillance and
mitigation planning.
The findings in this report are subject to at least three limitations. First, an absence
of reported outbreaks in some settings should not be interpreted as an absence of
COVID-19 cases in these settings, because local and tribal health departments in Wisconsin
directed limited resources to investigate outbreaks in high-risk congregate settings.
Therefore, lower-risk settings might be underrepresented. Second, local and tribal
health departments could not verify epidemiologic linkages for all cases in all outbreaks,
and some outbreak-associated cases could have occurred in other settings not represented
in this analysis. Finally, use of these surveillance data alone cannot determine whether
outbreaks in one setting are directly responsible for increases in community transmission
or outbreaks in other settings; more detailed epidemiologic or genomic data are needed
to explore whether such temporal correlations are causally related.
Examining trends in COVID-19 outbreaks over time provides an important indicator of
COVID-19 incidence across sectors in response to changing behaviors and policies.
State, local, and tribal health departments should continue to collect and report
such information, particularly among highly affected sectors such as long-term care
facilities and correctional facilities. Further, given the importance of college and
university outbreaks as potential early indicators of outbreaks in other settings,
colleges and universities should work with public health officials to strengthen surveillance
and mitigation strategies to prevent COVID-19 transmission.
Summary
What is already known about this topic?
COVID-19 incidence grew sharply in Wisconsin during September–November 2020; however,
the underlying cause of this rapid growth is unknown.
What is added by this report?
An examination of COVID-19 outbreaks in Wisconsin showed that cases linked to outbreaks
on college and university campuses increased sharply in August 2020 and were followed
by outbreaks in other high-risk congregate settings. Overall, outbreaks at long-term
care facilities (26.8%), correctional facilities (14.9%), and colleges or universities
(15.0%) accounted for the largest numbers of outbreak-associated cases in Wisconsin.
What are the implications for public health practice?
COVID-19 surveillance and mitigation planning should be prioritized for highly affected
settings such as long-term care facilities, correctional facilities, and colleges
and universities, which could represent early indicators of broader community transmission.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
COVID-19 Among Workers in Meat and Poultry Processing Facilities ― 19 States, April 2020
Jonathan W. Dyal, Michael Grant, Kendra Broadwater … (2020)
- Record: found
- Abstract: found
- Article: found
Multiple COVID-19 Clusters on a University Campus — North Carolina, August 2020
Erica Wilson, Catherine Donovan, Margaret Campbell … (2020)

- Record: found
- Abstract: found
- Article: found
Opening of Large Institutions of Higher Education and County-Level COVID-19 Incidence — United States, July 6–September 17, 2020
Andrew Leidner, Vaughn Barry, Virginia B Bowen … (2021)