- Record: found
- Abstract: found
- Article: found
Laparoscopic elective cholecystectomy with and without drain: A controlled randomised trial
Read this article at
Abstract
BACKGROUND:
Laparoscopic cholecystectomy is the main method of treatment of symptomatic gallstones. Routine drainage after laparoscopic cholecystectomy is an issue of considerable debate. Therefore, a controlled randomised trial was designed to assess the value of drains in elective laparoscopic cholecystectomy.
MATERIALS AND METHODS:
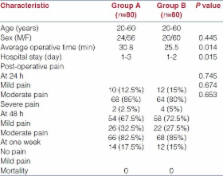
During a two-year period (From April 2008 to January 2010), 80 patients were simply randomised to have a drain placed (group A), an 8-mm pentose tube drain was retained below the liver bed, whereas 80 patients were randomised not to have a drain (group B) placed in the subhepatic space. End points of this trial were to detect any differences in morbidity, postoperative pain, wound infection and hospital stay between the two groups.
RESULTS:
There was no mortality in either group and no statistically significant difference in postoperative pain, nausea and vomiting, wound infection or abdominal collection between the two groups. However, hospital stay was longer in the drain group than in group without drain and it is appearing that the use of drain delays hospital discharge.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy.
- Record: found
- Abstract: found
- Article: not found
Effect of drainage on postoperative nausea, vomiting, and pain after laparoscopic cholecystectomy.
- Record: found
- Abstract: found
- Article: not found