- Record: found
- Abstract: found
- Article: found
Lateral Femoral Bowing and the Location of Atypical Femoral Fractures
Read this article at
Abstract
Purpose
Atypical femoral fractures (AFFs) occur in two distinct part, subtrochanter and diaphysis. The aim of this study was to investigate the relationship between the lateral femoral bowing angle and the location of AFF.
Materials and Methods
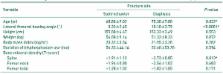
This study included a total of 56 cases in 45 patients who underwent surgical treatment between January 2010 and December 2015. For the diaphyseal and subtrochanteric AFFs, we evaluated the relationship between the anatomic location and lateral femoral bowing angle. Lateral femoral bowing angle was measured by two orthopaedic surgeons and average value of two calibrators was used in statistic analysis. Other variables like age, height, weight, body mass index and bone mineral density were also evaluated. We also calculated the cutoff value for the location of the fractures from the raw data.
Results
The average lateral femoral bowing angle was 10.10°±3.79° (3°-19°) in diaphyseal group and 3.33°±2.45° (1.5°-11°) in subtrochanter group. Lateral femoral bowing angle was statistically significant in logistic regression analysis. According to the receiver operating characteristic curve, cutoff value for the location of the fracture was 5.25°. In other words, the femoral diaphyseal fractures are more frequent if the lateral femoral bowing angle is greater than 5.25°.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research.
- Record: found
- Abstract: found
- Article: not found