- Record: found
- Abstract: found
- Article: not found
Electrical Storm in a Febrile Patient with Brugada Syndrome and COVID-19 Infection
case-report
Andrew Aboyme , M.D,
Bobby D. Ghosh , M.D,
Sabha Bhatti , M.D,
William J. Kostis , Ph.D., M.D,
Theodore J. Maglione , M.D
∗
17 July 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Introduction
The eponymous syndrome first described by the Brugada brothers in the early 1990s
consists of characteristic ST abnormalities and an increased risk of sudden cardiac
death due to ventricular arrhythmias.1 Since that time, further genetic research has
implicated hundreds of variants in 17 genes with mutations in SCN5A, coding for voltage-gated
sodium channels, accounting for the majority of genotyped patients.2 Various triggers
have been associated with the development of ventricular fibrillation (VF) in this
patient population including fever and alcohol intake.3
We present a case of electrical storm in the setting of acute febrile illness in a
patient with Burgada syndrome and COVID-19 infection.
Case Report
A 58-year-old woman with a history of hypertension, diabetes mellitus, and Brugada
syndrome for which she underwent implantable cardioverter defibrillator (ICD) implantation
in 2017, presented following a 3-day febrile illness and, on the day of presentation,
multiple syncopal episodes. She had previously had a syncopal episode in 2019 that
occurred in the setting of ventricular fibrillation (VF) that was terminated by a
single shock from her device.
Interrogation of her ICD in the emergency department revealed multiple episodes of
ventricular fibrillation (VF), some of which were non-sustained, as well as 7 episodes
that were terminated by appropriate ICD shocks. The fever persisted after admission
despite the use of antipyretics with a maximum temperature of 101.7 °F in the first
24 hours. During these febrile periods, she continued to have additional episodes
of VF requiring shock termination (Figure 1
). Rapid nasal swab testing in the emergency department was positive for severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2) and prompted admission to the ICU.
Isoproterenol infusion (2 mcg bolus followed by 1 mcg/min) was initiated as well as
aggressive treatment of the fever with standing acetaminophen and salsalate. Despite
these measures, the fever persisted and additional temperature management with a cooling
blanket was needed for fever control. She did not have any further ventricular arrhythmias
after her temperature normalized (Figure 2
).
Figure 1
One of multiple episodes of ventricular fibrillation requiring shock termination in
the patient while febrile due to COVID-19 infection. Of note is the coved-type ST
pattern appreciated in V1.
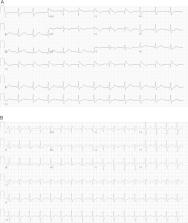
Figure 2
Dynamic change in Brugada pattern with treatment. A. Twelve-lead electrocardiogram
(ECG) obtained soon after presentation. B. ECG obtained following control of the patient’s
fever and administration of isoproterenol.
She was started on hydroxychloroquine on hospital day 1, however it was discontinued
the following day due to QTc prolongation to 554 ms. Oxygenation proved difficult,
and her respiratory status continued to decline despite the use of a non-rebreather
mask and prone positioning. While her initial chest radiograph was unremarkable, serial
radiographs revealed development of multifocal airspace and interstitial opacities
consistent with acute respiratory distress syndrome from COVID-19 associated pneumonia.
On hospital day 3, isoproterenol was discontinued due to several sustained episodes
of atrial tachycardia with rates of 140-150 beats/minute. Broad-spectrum antibiotics
were started on hospital day 5 due to concern for possible superimposed bacterial
pneumonia. Remdesivir was initiated on hospital day 6, however her respiratory function
continued to decline, requiring intubation. During her hospital course, she developed
laboratory evidence of severe disease with progressive lymphopenia (130/μL) and increased
CRP (54.5 mg/dL), D-dimer (8474 ng/mL), fibrinogen (>1000 mg/dL), ferritin (1116 ng/mL),
and procalcitonin (2.7 ng/mL). She was started on therapeutic anticoagulation with
LMWH due to her hypercoagulable state.
She continued to decline with the development of septic shock requiring initiation
of multiple vasopressors. Although she had infrequent episodes of atrial tachycardia,
she had no further ventricular arrhythmias. During a sedation holiday on hospital
day 18, she was noted to be unarousable. CT imaging revealed extensive intracranial
hemorrhage with resultant mass effect. Given her severe and irreversible neurological
injury, her family members decided to transition to comfort care.
Discussion
Brugada syndrome typically presents during adulthood with a mean age of sudden cardiac
death occurring at 41 ± 15 years old.4 Abnormalities in SCN5A, a gene which encodes
the α-subunit of cardiac sodium channels, remains the most common genotype. Mutation
in this channel results in loss of sodium channel function with resultant delay in
phase 0 action potential upstroke and slowing of conduction.5 The ventricular arrhythmias
that develop in this patient population can be highly lethal. For this reason, ICDs
are recommended for patients who are survivors of cardiac arrest and/or have documented
spontaneous VT/VF, as well as those with other high-risk features.6
While Brugada syndrome has been well studied over the past several decades, COVID-19
is a relatively new entity. In early December 2019, the first cases of SARS-CoV-2
were identified in Wuhan, China.7 In the following months, the virus spread throughout
the world, posing a significant global challenge to combat the pandemic. One of the
most common symptoms in COVID-19 infection is fever, which is present in 83-99% of
patients.8 It is well known that a subset of COVID-19 patients will develop cytokine
storm. This is a clinical entity characterized with high and unrelenting fevers, often
with temperatures >39.4 °C.9 We believe our patient to have developed secondary cytokine
storm which underscores the importance of temperature control in patients with Brugada
syndrome and COVID-19 infection. In many patients it is not until fever is present
that a Type I ECG pattern becomes apparent, which itself carries an increased risk
of fatal arrhythmias.10 It is believed that at increased temperatures sodium channel
gating is augmented in patients with SCN5A mutations resulting in altered net outward
current during right ventricular depolarization.11 This relationship of fever unmasking
electrocardiographic changes has been described in the COVID population.12
Electrical storm is the highly feared electrophysiologic sequelae of Brugada syndrome.
As fever precipitates ventricular arrhythmias in Brugada syndrome this concern is
particularly amplified in patients with COVID-19 infection, a condition characterized
by high fever curves.13 Acute management of electrical storm in Brugada syndrome with
COVID infection includes treating any arrhythmic triggers, such as the utilization
of acetaminophen for fever control.14 If antipyretics prove ineffective, our recommendation
would be to use other non-pharmacologic measures such as cooling blankets, packed
ice, or even cooling catheters normally reserved for therapeutic hypothermia protocols.
Other data has demonstrated benefit to isoproterenol infusion in the treatment of
electrical storm (administered as a bolus injection of 1–2 mcg followed by continuous
infusion at a dose of 0.15–2.0 mcg/min to maintain a 20% increase in heart rate).
A nonspecific β-agonist, isoproterenol increases heart rate and has been shown to
decrease J-point amplitude, change coved-type to saddleback-type ST-segment patterns,
and even normalize ST-segment elevation, thereby suppressing VF.15 Quinidine is a
class Ia antiarrhythmic agent that can be used in treatment of electrical storm in
the Brugada population. It possesses anticholinergic effects and results in the inhibition
of Ito in the ventricular epicardium to help suppress VF. Given the benefit of these
medications, they are recommended by both American and European societies for the
treatment of electrical storm.
6
,16 In our patient, the combination of antipyretic therapy and isoproterenol infusion
was successful in suppressing ventricular arrhythmias.
Conclusion
This case describes the development of electrical storm in a patient with Brugada
syndrome in the setting of an acute febrile illness due to COVID-19 infection. In
addition to aggressively controlling her fever, isoproterenol was required for suppression
of ventricular arrhythmias. While there is an established association between fever
and ventricular arrhythmias in patients with Brugada syndrome
9
, the presence of prolonged high-grade fever in those infected with COVID-19 may pose
additional risks in these patients.
Key Teaching Points
1.
COVID-19 infection often presents with high fever. Among severely ill COVID-19 patients,
some develop secondary cytokine storm syndromes characterized by high and unremitting
fever.
2.
Patients in this population with underlying Brugada syndrome are at particular risk
of adverse outcomes due to the known association of fever and ventricular arrhythmias.
3.
The prompt recognition and treatment of fevers and arrhythmias in patients with Brugada
syndrome and COVID-19 infection is crucial for favorable outcomes.
Uncited reference
1, 2, 3, 4, 5, 7, 8, 10, 11, 12, 13, 14, 15, 16.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics of Coronavirus Disease 2019 in China
Wei-jie Guan, Zheng-yi Ni, Yu Hu … (2020)
- Record: found
- Abstract: found
- Article: found
COVID-19: consider cytokine storm syndromes and immunosuppression
Puja Mehta, Daniel McAuley, Michael Brown … (2020)
- Record: found
- Abstract: found
- Article: not found
