- Record: found
- Abstract: found
- Article: found
Detection of Reduced Diameter of the Cochlear Nerve in Long-term Deaf Patients Quantified With Semiautomatic Measurement of Nerve Cross-sectional Area Using 3T MRI Data
Read this article at
Abstract
Hypothesis:
High-resolution parallel transmit T2 sampling perfection with application optimized contrast using different flip angle evolution sequence with improved edge discrimination and semiautomatic determination of nerve cross-sectional area (CSA) can be used to evaluate nerve degeneration in the inner auditory canal (IAC) in long-term deaf patients.
Background:
In patients with hearing loss, temporal bone MRI is routinely acquired to evaluate the morphology of the nerves within the IAC. Earlier studies have shown that the diameter of the cochlear nerve can be used as prognostic marker for the auditory performance after cochlear implantation in postlingually deaf patients.
Methods:
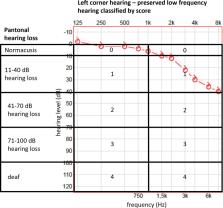
Eighty-two consecutive MRI scans were analyzed using a semiautomatic tool to measure CSA of cranial nerves in the IAC. Results were correlated with patient history and audiology testing as well as with age and gender.
Results:
There was a significant reduced CSA of the cochlear nerve in ears with moderate-to-profound hearing loss and deafness compared with ears with normal hearing, but no significant difference in ears with mild-to-moderate hearing loss compared with normal hearing. In detail, normal hearing ears had a CSA of 1.23 ± 0.11 mm 2, whereas ears with pantonal hearing loss of more than 40 dB had 1.02 ± 0.05 mm 2 ( P = 0.026). Maximal CSA of the facial nerve was not different among all groups (average, 1.04 mm 2 ± 0.03; linear regression, P = 0.001) and stable with age. However, vestibular nerve CSA decreased significantly with age (average, 1.78 ± 0.05 mm 2; linear regression, P = 0.128).
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Diameter of the cochlear nerve in deaf humans: implications for cochlear implantation.
- Record: found
- Abstract: found
- Article: not found
Electrophysiologic and behavioral outcomes of cochlear implantation in children with auditory nerve hypoplasia.
- Record: found
- Abstract: found
- Article: not found