- Record: found
- Abstract: found
- Article: found
Transcranial doppler sonography is not a valid diagnostic tool for detection of basilar artery stenosis or in-stent restenosis: a retrospective diagnostic study
Read this article at
Abstract
Background
There are contradictory reports concerning the validity of transcranial sonography (TCD and TCCS) for examinations of the basilar artery. Here we investigated sensitivity and specificity of transcranial sonography for the detection of basilar artery stenosis and in-stent-restenosis compared to cerebral angiography.
Methods
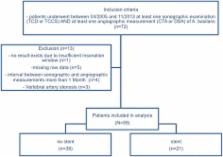
We analyzed data of 104 examinations of the basilar artery. The association between sonographic peak systolic velocity (PSV) and degree of stenosis obtained by cerebral angiography was evaluated applying Spearman’s correlation coefficient. Receiver Operating Characteristics (ROC) curves and areas under the curve (AUC) were calculated for the detection of a ≥50% stenosis defined by angiography. Optimal cut-off was derived using the Youden-index.
Results
A weak but statistically significant correlation between PSV and the degree of stenosis was found ( n=104, rho=0.35, p<0.001). ROC analysis for a detection of ≥50% stenosis showed an AUC of 0.70, a sensitivity of 74.0% and a specificity of 65.0% at the optimal cut off of 124 cm/s. Results were consistent when analyzing examinations done in stented and unstented arteries separately (TCD VS DSA/CTA in unstented artery: AUC=0.66, sensitivity 61.0%, specificity 65.0%, TCD/TCCS VS DSA in stented artery: AUC=0.63, sensitivity 71.0%, specificity 82.0%). Comparing TCCS measurements exclusively to angiography, ROC analysis showed an AUC of 1.00 for the detection of an in-stent-restenosis ≥50% with a sensitivity and specificity of 100% when a PSV of 132 cm/s was used as a cut off value.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: found
Twisted Blood Vessels: Symptoms, Etiology and Biomechanical Mechanisms
- Record: found
- Abstract: found
- Article: not found
Intracranial vascular stenosis and occlusive disease: evaluation with CT angiography, MR angiography, and digital subtraction angiography.
- Record: found
- Abstract: found
- Article: not found