- Record: found
- Abstract: found
- Article: found
Systemic Sclerosis With a Normotensive Scleroderma Renal Crisis: A Diagnostic Dilemma
Read this article at
Abstract
Systemic sclerosis (SSc), also called scleroderma, is an auto-immune rheumatic disease that is characterized by fibrosis of the skin and internal organs and vasculopathy. Three of the severe manifestations of the disease include a scleroderma renal crisis (SRC), pulmonary arterial hypertension, and digital ulceration. Vascular manifestations like Raynaud's phenomenon are an almost universal symptom in patients with SSc and are often the earliest manifestation of the disease.
An SRC occurs in approximately 10% of all patients with scleroderma. It is characterized by malignant hypertension and progressive renal failure. However, about 10% of SRC cases present with normal blood pressure or a normotensive renal crisis.
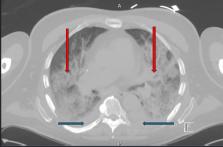
A 65-year-old man with a history of peripheral vascular disease and newly diagnosed heart failure presented to the emergency department on account of progressive discoloration of the left big toe and intermittent confusion. Initially, he was noted to be hemodynamically stable, with bluish discoloration of his left lower extremity and left big toe, which was tender to palpation with palpable distal pulses. His left toe progressively became dusky and gangrenous, necessitating ray amputation by vascular surgery. His hospital course was further complicated by worsening acute kidney injury, requiring initiation of hemodialysis, and progressive hypoxia with the transition from room air to high-flow oxygen. As part of his workup for acute kidney injury (AKI), his antinuclear antibody (ANA) was found to be positive, with high titers, as well as elevated SCl-70 IgG. Despite the initiation of hemodialysis, and post-surgical revision, he continued to deteriorate. His family opted for comfort care measures, and he died a few days later.
Although SSc is a rare disease, it is associated with significant morbidity and has one of the highest mortality rates among connective tissue diseases. SSc can present with heterogeneous manifestations, mimicking several isolated organ-specific conditions. This makes the diagnosis challenging, especially early in the course of the disease. A high index of suspicion, especially in the setting of rapidly progressing multi-organ involvement without a clear cause, should prompt further evaluation of systemic sclerosis.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative.
- Record: found
- Abstract: found
- Article: not found
Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database.
- Record: found
- Abstract: found
- Article: not found