- Record: found
- Abstract: found
- Article: found
The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review
Read this article at
Abstract
Background: Providing information that is congruent with patients’ needs is an important determinant for patient satisfaction and might also affect health-related quality of life (HRQoL) and anxiety and depression levels of cancer survivors.
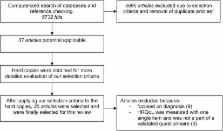
Design: The authors systematically reviewed the available literature on the relationship between information provision and HRQoL, anxiety and depression. A PubMed literature search for original articles published until February 2010 was carried out. Twenty-five articles, all conducted between 1996 and 2009, which met the predefined inclusion criteria, were subjected to a quality checklist.
Results: Satisfied patients, patients with fulfilled information needs, and patients who experience less information barriers, in general have a better HRQoL and less anxiety and depression. Out of eight intervention studies that aimed to improve information provision, only one showed a positive association with better HRQoL.
Conclusion: Health care providers must pay more attention to patient-centred information provision. Additional research is needed to make definitive conclusions about information interventions as most results did not reach statistical significance due to methodological constraints. The quick development of the relatively young research field of patient-reported outcomes in cancer survivorship will make it possible to conduct better quality studies in the future.
Related collections
Most cited references42
- Record: found
- Abstract: found
- Article: not found
What are the unmet supportive care needs of people with cancer? A systematic review.
- Record: found
- Abstract: found
- Article: not found
Quality of life among long-term breast cancer survivors: a systematic review.
- Record: found
- Abstract: found
- Article: not found