- Record: found
- Abstract: found
- Article: found
Lymphocytic esophagitis: Report of three cases and review of the literature
Read this article at
Abstract
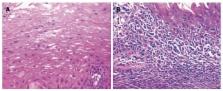
Lymphocytic esophagitis (LyE) is a rare condition characterised histologically by high numbers of esophageal intraepithelial lymphocytes without significant granulocytes infiltration, in addition to intercellular edema (“spongiosis”). The clinical significance and natural history of LyE is poorly defined although dysphagia is reportedly the most common symptom. Endoscopic features range from normal appearing esophageal mucosa to features similar to those seen in eosinophilic esophagitis, including esophageal rings, linear furrows, whitish exudates, and esophageal strictures/stenosis. Symptomatic gastroesophageal reflux disease is an inconsistent association. LyE has been associated in paediatric Crohn’s disease, and recently in primary esophageal dysmotility disorder in adults. There are no studies assessing effective treatment strategies for LyE; empirical therapies have included use of proton pump inhibitor and corticosteroids. Esophageal dilatation have been used to manage esophageal strictures. LyE has been reported to run a benign course; however there has been a case of esophageal perforation associated with LyE. Here, we describe the clinical, endoscopic and histopathological features of three patients with lymphocytic esophagitis along with a review of the current literature.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis.
- Record: found
- Abstract: found
- Article: not found
Budesonide is effective in treating lymphocytic colitis: a randomized double-blind placebo-controlled study.
- Record: found
- Abstract: found
- Article: not found