- Record: found
- Abstract: found
- Article: found
The Importance of DS-14 and HADS Questionnaires in Quantifying Psychological Stress in Type 2 Diabetes Mellitus
Read this article at
Abstract
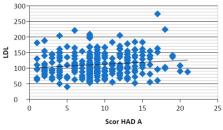
Background and Objectives: The comorbid association between type 2 diabetes mellitus (T2DM) and a psychological profile characterized by depression and/or anxiety has been reported to increase the risk of coronary heart disease (CAD), the most striking macrovascular complication of diabetes. The purpose of the present study was to quantify anxiety, depression and the presence of type D personality, and to correlate the scores obtained with cardiovascular risk factors and disease severity in diabetic patients. Materials and methods: The retrospective study included 169 clinically stable diabetic patients divided into two groups: group 1 without macrovascular complications ( n = 107) and group 2 with CAD, stroke and/or peripheral vascular disease ( n = 62). A biochemical analysis and an assessment of psychic stress by applying the Hospital Anxiety and Depression Scale (HADS)and the Type D scale (DS-14) to determine anxiety, depression and D personality scores were done in all patients. Statistical analysis was made using SPSSv17 and Microsoft Excel, non-parametric Kruskal–Wallis and Mann–Whitney tests. Results: Following application of the HAD questionnaire for the entire group ( n = 169), anxiety was present in 105 patients (62.2%), and depression in 96 patients (56.8%). Group 2 showed significantly higher anxiety scores compared to group 1 ( p = 0.014), while depression scores were not significantly different. Per entire group, analysis of DS-14 scores revealed social inhibition (SI) present in 56 patients (33%) and negative affectivity (NA) in 105 patients (62%). TheDS-14 SI score was significantly higher in group 2 compared to group 1 ( p = 0.036). Type D personality, resulting from scores above 10 in both DS-14 parameter categories, was present in 51 patients of the study group (30%). There was a direct and significant correlation ( r = 0.133, p = 0.025) between the Hospital Anxiety and Depression Scale-Anxiety (HAD-A) score and the LDL-c values. Conclusions: The results of this study demonstrated that more than a half of patients with diabetes had anxiety and/or depression and one third had Type D personality, sustaining that monitoring of emotional state and depression should be included in the therapeutic plan of these patients. New treatment strategies are needed to improve the well-being of diabetic patients with psychological comorbidities.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Diabetes and depression.
- Record: found
- Abstract: found
- Article: found
The association between Diabetes mellitus and Depression
- Record: found
- Abstract: found
- Article: found