- Record: found
- Abstract: found
- Article: found
Inflammatory cytokines as mediators of retinal endothelial barrier dysfunction in non‐infectious uveitis

Read this article at
Abstract
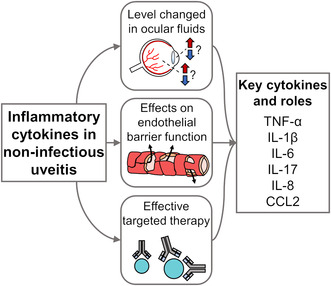
Characterised by intraocular inflammation, non‐infectious uveitis includes a large group of autoimmune and autoinflammatory diseases that either involve the eye alone or have both ocular and systemic manifestations. When non‐infectious uveitis involves the posterior segment of the eye, specifically the retina, there is substantial risk of vision loss, often linked to breakdown of the inner blood‐retinal barrier. This barrier is formed by non‐fenestrated retinal vascular endothelial cells, reinforced by supporting cells that include pericytes, Müller cells and astrocytes. Across the published literature, a group of inflammatory cytokines stand out as prominent mediators of intraocular inflammation, with effects on the retinal endothelium that may contribute to breakdown of the inner blood‐retinal barrier, namely tumour necrosis factor (TNF)‐α, interleukin (IL)‐1β, IL‐6, IL‐8, IL‐17 and chemokine C‐C motif ligand (CCL)2. This article reviews the function of each cytokine and discusses the evidence for their involvement in retinal endothelial barrier dysfunction in non‐infectious uveitis, including basic laboratory investigations, studies of ocular fluids collected from patients with non‐infectious uveitis, and results of clinical treatment trials. The review also outlines gaps in knowledge in this area. Understanding the disease processes at a molecular level can suggest treatment alternatives that are directed against appropriate biological targets to protect the posterior segment of eye and preserve vision in non‐infectious uveitis.
Abstract
Non‐infectious uveitis has a range of ocular and systemic autoimmune and autoinflammatory causes. When the retina is involved, blood‐retinal barrier breakdown can lead to vision loss. Specific cytokines stand out as promoting intraocular inflammation. This article reviews the involvement of inflammatory cytokines – including tumour necrosis factor (TNF)‐α, interleukin (IL)‐1β, IL‐6, IL‐8, IL‐17 and chemokine C‐C motif ligand (CCL)2 – in non‐infectious uveitis. Their levels in ocular fluids, their effects on the endothelial barrier, and the results of clinical treatment trials are discussed.
Related collections
Most cited references259
- Record: found
- Abstract: found
- Article: not found
Standardization of Uveitis Nomenclature for Reporting Clinical Data. Results of the First International Workshop
- Record: found
- Abstract: found
- Article: not found