- Record: found
- Abstract: found
- Article: found
Bullous Henoch-Schönlein Purpura and Associated Nephritis: A Pathological Case Report
Read this article at
Abstract
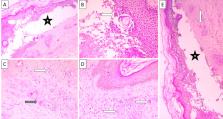
Henoch-Schönlein purpura (HSP) is the most common vasculitis in childhood, presenting with purpura, predominantly of the lower extremities and occasionally with renal involvement as well. Although associated with childhood, HSP, although rarely, can also develop in adults as well. Here we present a patient in his sixties, presenting with a myriad of rash units on his lower extremities, including bullous ones, and a constellation of chronic kidney failure. Skin and renal biopsy specimens revealed morphological changes and immune depositions representative of HSP. Despite treatment, the patient's kidney failure slowly progressed, and he expired eight months after his presentation due to associated complications. Although rare, the bullous form of HSP can be viewed as a more aggressive form of the disease, as seen by the presentation constellation and rapid progression in our case.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins.
- Record: found
- Abstract: found
- Article: not found
Risk of long term renal impairment and duration of follow up recommended for Henoch-Schonlein purpura with normal or minimal urinary findings: a systematic review.
- Record: found
- Abstract: found
- Article: not found