- Record: found
- Abstract: found
- Article: found
SARS‐CoV‐2 infection in pregnancy during the first wave of COVID‐19 in the Netherlands: a prospective nationwide population‐based cohort study (NethOSS)
Read this article at
Abstract
Objective
To describe characteristics, risk factors and maternal, obstetric and neonatal outcomes of pregnant women infected with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2).
Population
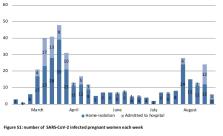
Pregnant women with confirmed SARS‐CoV‐2 infection admitted to hospital or in home‐isolation: 1 March 2020 to 31 August 2020.
Methods
Pregnant women with positive polymerase chain reaction or antibody tests were registered using the Netherlands Obstetrics Surveillance System (NethOSS). (Selective) testing occurred according to national guidelines. Data from the national birth registry (pregnant pre‐coronavirus disease 2019 [COVID‐19] cohort) and an age‐matched cohort of COVID‐19‐positive women (National Institute for Public Health and the Environment; fertile age COVID‐19 cohort) were used as reference.
Main outcome measures
Incidence of SARS‐CoV‐2 infection in pregnant women. Maternal, obstetric and neonatal outcomes including hospital and intensive care admission.
Results
Of 376 registered pregnant women with confirmed SARS‐CoV‐2 infection, 20% (74/376) were admitted to hospital, of whom 84% (62/74) were due to SARS‐CoV‐2; 10% (6/62) were admitted to intensive care and 15% (9/62) to obstetric high‐care units. Risk factors for admission were non‐European country of origin (odds ratio [OR] 1.73, 95% CI 1.01–2.96) and being overweight/obese (OR 1.86, 95% CI 1.51–3.20). No maternal or perinatal deaths occurred. Caesarean section after labour‐onset was increased (OR 1.58, 95% CI 1.09–2.28). Hospital and intensive care admission were higher compared with the fertile age COVID‐19 cohort (OR 6.75, 95% CI 5.18–8.81 and OR 2.52, 95% CI 1.11–5.77, respectively).
Tweetable abstract
Pregnant women with SARS‐CoV‐2 in the Netherlands show increased hospital/ICU admission and caesarean section.
Related collections
Most cited references28

- Record: found
- Abstract: found
- Article: found
Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study

- Record: found
- Abstract: found
- Article: found
Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis

- Record: found
- Abstract: found
- Article: found