- Record: found
- Abstract: found
- Article: found
Comparing the Osteogenic Potentials and Bone Regeneration Capacities of Bone Marrow and Dental Pulp Mesenchymal Stem Cells in a Rabbit Calvarial Bone Defect Model
Read this article at
Abstract
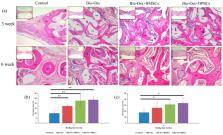
The bone regeneration efficiency of bone marrow mesenchymal stem cells (BMSCs) and dental pulp mesenchymal stem cells (DPSCs) combined with xenografts in the craniofacial region remains unclear. Accordingly, this study commenced by comparing the cell morphology, cell proliferation, trilineage differentiation, mineral synthesis, and osteogenic gene expression of BMSCs and DPSCs in vitro. Four experimental groups (empty control, Bio-Oss only, Bio-Oss+BMSCs, and Bio-Oss+DPSCs) were then designed and implanted in rabbit calvarial defects. The BMSCs and DPSCs showed a similar morphology, proliferative ability, surface marker profile, and trilineage-differentiation potential in vitro. However, the BMSCs exhibited a higher mineral deposition and expression levels of osteogenic marker genes, including alkaline phosphatase (ALP), runt related transcription factor 2 (RUNX2), and osteocalcin (OCN). In the in vivo studies, the bone volume density in both MSC groups was significantly greater than that in the empty control or Bio-Oss only group. Moreover, the new bone formation and Collagen I / osteoprotegerin protein expressions of the scaffold+MSC groups were higher than those of the Bio-Oss only group. Finally, the Bio-Oss+BMSC and Bio-Oss+DPSC groups had a similar bone mineral density, new bone formation, and osteogenesis-related protein expression. Overall, the DPSCs seeded on Bio-Oss matched the bone regeneration efficacy of BMSCs in vivo and hence appear to be a promising strategy for craniofacial defect repair in future clinical applications.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Mesenchymal stem cells: mechanisms of inflammation.
- Record: found
- Abstract: found
- Article: not found
Concise reviews: Characteristics and potential applications of human dental tissue-derived mesenchymal stem cells.

- Record: found
- Abstract: found
- Article: found