- Record: found
- Abstract: found
- Article: found
Reduced postoperative pain using Nociception Level-guided fentanyl dosing during sevoflurane anaesthesia: a randomised controlled trial
Read this article at
Abstract
Background
The majority of postoperative patients report moderate to severe pain, possibly related to opioid underdosing or overdosing during surgery. Objective guidance of opioid dosing using the Nociception Level (NOL) index, a multiparameter artificial intelligence-driven index designed to monitor nociception during surgery, may lead to a more appropriate analgesic regimen, with effects beyond surgery. We tested whether NOL-guided opioid dosing during general anaesthesia results in less postoperative pain.
Methods
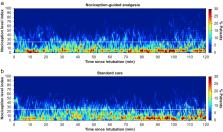
In this two-centre RCT, 50 patients undergoing abdominal surgery under fentanyl/sevoflurane anaesthesia were randomised to NOL-guided fentanyl dosing or standard care in which fentanyl dosing was based on haemodynamics. The primary endpoint of the study was postoperative pain assessed in the PACU.
Results
Median postoperative pain scores were 3.2 (inter-quartile range 1.3–4.3) and 4.8 (3.0–5.3) in NOL-guided and standard care groups, respectively ( P=0.006). Postoperative morphine consumption (standard deviation) was 0.06 (0.07) mg kg −1 (NOL-guided group) and 0.09 (0.09) mg kg −1 (control group; P=0.204). During surgery, fentanyl dosing was not different between groups (NOL-guided group: 6.4 [4.2] μg kg −1 vs standard care: 6.0 [2.2] μg kg −1, P=0.749), although the variation between patients was greater in the NOL-guided group (% coefficient of variation 66% in the NOL-guided group vs 37% in the standard care group).
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis.

- Record: found
- Abstract: found
- Article: found
Poorly controlled postoperative pain: prevalence, consequences, and prevention
- Record: found
- Abstract: found
- Article: not found