- Record: found
- Abstract: found
- Article: found
Viral reactivations and co-infections in COVID-19 patients: a systematic review
Read this article at
Abstract
Background
Viral reactivations and co-infections have been reported among COVID-19 patients. However, studies on the clinical outcomes of different viral reactivations and co-infections are currently in limit. Thus, the primary purpose of this review is to perform an overarching investigation on the cases of latent virus reactivation and co-infection in COVID-19 patients to build collective evidence contributing to improving patient health. The aim of the study was to conduct a literature review to compare the patient characteristics and outcomes of reactivations and co-infections of different viruses.
Methods
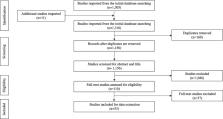
Our population of interest included confirmed COVID-19 patients who were diagnosed with a viral infection either concurrently or following their COVID-19 diagnosis. We extracted the relevant literature through a systematic search using the key terms in the online databases including the EMBASE, MEDLINE, Latin American Caribbean Health Sciences Literature (LILACS), from inception onwards up to June 2022. The authors independently extracted data from eligible studies and assessed the risk of bias using the Consensus-based Clinical Case Reporting (CARE) guidelines and the Newcastle–Ottawa Scale (NOS). Main patient characteristics, frequency of each manifestation, and diagnostic criteria used in studies were summarized in tables.
Results
In total, 53 articles were included in this review. We identified 40 reactivation studies, 8 coinfection studies, and 5 studies where concomitant infection in COVID-19 patients was not distinguished as either reactivation or coinfection. Data were extracted for 12 viruses including IAV, IBV, EBV, CMV, VZV, HHV-1, HHV-2, HHV-6, HHV-7, HHV-8, HBV, and Parvovirus B19. EBV, HHV-1, and CMV were most frequently observed within the reactivation cohort, whereas IAV and EBV within the coinfection cohort. In both reactivation and coinfection groups, patients reported cardiovascular disease, diabetes, and immunosuppression as comorbidities, acute kidney injury as complication, and lymphopenia and elevated D-dimer and CRP levels from blood tests. Common pharmaceutical interventions in two groups included steroids and antivirals.
Related collections
Most cited references107

- Record: found
- Abstract: found
- Article: found
The PRISMA 2020 statement: an updated guideline for reporting systematic reviews
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study

- Record: found
- Abstract: found
- Article: found