- Record: found
- Abstract: found
- Article: found
HPV self-sampling acceptability in rural and indigenous communities in Guatemala: a cross-sectional study
Read this article at
Abstract
Introduction
Cervical cancer disproportionately burdens low-income and middle-income countries (LMICs) such as Guatemala. Self-collection testing for human papillomavirus (HPV) has been suggested as a form of cervical cancer screening to facilitate access in LMICs. This study assessed and compared the acceptability of self-collection HPV testing in two rural, indigenous and ethnically distinct communities in Guatemala: Santiago Atitlán, Sololá and Livingston, Izabal.
Methods
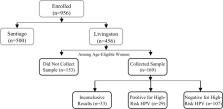
All participants, women between the ages of 18 and 60, completed a questionnaire. Eligible participants were also asked to self-collect a vaginal sample and complete a questionnaire regarding comfort and acceptability. Self-collected samples were tested for high-risk HPV using the real-time PCR Hybribio kit.
Results
In the indigenous community of Santiago Atitlán, of 438 age-eligible participants, 94% completed self-collection. Of those, 81% found it comfortable and 98% were willing to use it as a form of screening. In the multiethnic (Afro-Caribbean, indigenous) community of Livingston, of 322 age-eligible participants, 53% chose to self-collect. Among those who took the test, 83% found it comfortable and 95% were willing to use it as a form of screening. In Livingston, literacy (can read and/or write vs cannot read or write) was higher in women who chose to self-collect (prevalence ratio 2.25; 95% CI 1.38 to 3.68). Ethnicity, history of screening and reproductive history were not associated with willingness to self-collect in Livingston. Women in Santiago reported less prior use of healthcare than women in Livingston. Overall, 19% (106/549) of samples tested positive for high-risk HPV.
Conclusion
Among women willing to self-collect in rural and indigenous communities in Guatemala, self-collection for HPV testing is highly acceptable. However, willingness to try self-collection might vary across communities and settings. Women from a community that used less healthcare were more likely to choose self-collection. Further research is necessary to determine what factors influence a woman’s choice to self-collect.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Screening for Cervical Cancer
- Record: found
- Abstract: found
- Article: not found