- Record: found
- Abstract: found
- Article: found
Patient-reported factors influencing the choice of their kidney replacement treatment modality
Read this article at
Abstract
Background
Access to various kidney replacement therapy (KRT) modalities for patients with end-stage kidney disease differs substantially within Europe.
Methods
European adults on KRT filled out an online or paper-based survey about factors influencing and experiences with modality choice (e.g. information provision, decision-making and reasons for choice) between November 2017 and January 2019. We compared countries with low, middle and high gross domestic product (GDP).
Results
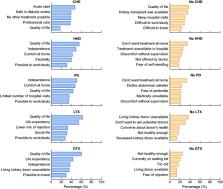
In total, 7820 patients [mean age 59 years, 56% male, 63% on centre haemodialysis (CHD)] from 38 countries participated. Twenty-five percent had received no information on the different modalities, and only 23% received information >12 months before KRT initiation. Patients were not informed about home haemodialysis (HHD) (42%) and comprehensive conservative management (33%). Besides nephrologists, nurses more frequently provided information in high-GDP countries, whereas physicians other than nephrologists did so in low-GDP countries. Patients from low-GDP countries reported later information provision, less information about other modalities than CHD and lower satisfaction with information. The majority of modality decisions were made involving both patient and nephrologist. Patients reported subjective (e.g. quality of life and fears) and objective reasons (e.g. costs and availability of treatments) for modality choice. Patients had good experiences with all modalities, but experiences were better for HHD and kidney transplantation and in middle- and high-GDP countries.
Conclusion
Our results suggest European differences in patient-reported factors influencing KRT modality choice, possibly caused by disparities in availability of KRT modalities, different healthcare systems and varying patient preferences. Availability of home dialysis and kidney transplantation should be optimized.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES)
- Record: found
- Abstract: found
- Article: not found
Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant.
- Record: found
- Abstract: found
- Article: not found