- Record: found
- Abstract: found
- Article: found
Effects of In-Person Assistance vs Personalized Written Resources About Social Services on Household Social Risks and Child and Caregiver Health : A Randomized Clinical Trial
Read this article at
Abstract
This randomized clinical trial examined the effect of in-person social services navigation assistance vs a written information sheet on caregiver-reported social risk factors and child and caregiver health.
Key Points
Question
Did in-person, longitudinal social services navigation assistance result in greater reduction in social risk factors and better health for children and caregivers than a less intensive approach?
Findings
In this randomized clinical trial including 611 caregiver-child dyads, there were no statistically significant differences between the groups in the effectiveness of the interventions. In post hoc secondary analyses of both groups, there were significant improvements in social risk factors and in child and caregiver health at 6-month follow-up.
Abstract
Importance
Social and economic contexts shape children’s short- and long-term health. Efforts to address contextual risk factors are increasingly incorporated into pediatric health care.
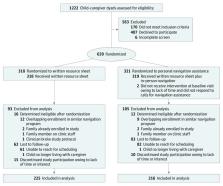
Design, Setting, and Participants
This randomized clinical trial included English- and/or Spanish-speaking caregiver-child dyads recruited from a pediatric urgent care clinic nested in a large, urban, safety-net hospital. Study recruitment, enrollment, and follow-up were conducted from July 18, 2016, to March 8, 2019. Data analysis was conducted from January 1, 2019, to January 20, 2020.
Interventions
Following standardized social risk assessment, caregivers were randomly assigned to receive either written information regarding relevant government and community social services resources or comparable written information plus in-person assistance and follow-up focused on service access.
Main Outcomes and Measures
Caregiver-reported number of social risk factors and child health 6 months after enrollment.
Results
Among 611 caregiver-child dyads enrolled in the study, 302 dyads were randomized to the written resources group and 309 dyads were randomized to the written resources plus in-person assistance group. The mean (SD) age of children was 6.1 (5.0) years; 483 children (79.1%) were Hispanic; and 315 children (51.6%) were girls. There were no significant differences between groups in the effects of the interventions. In post hoc secondary analyses, the number of reported social risks decreased from baseline to 6-month follow-up in both groups: caregivers who received written resources alone reported a mean (SE) of 1.28 (0.19) fewer risks at follow-up, while those receiving written resources plus in-person assistance reported 1.74 (0.21) fewer risks at follow-up (both P < .001). In both groups, there were small but statistically significant improvements from baseline to follow-up in child health (mean [SE] change: written resources, 0.37 [0.07]; written resources plus in-person assistance, 0.24 [0.07]; both P < .001).
Conclusions and Relevance
This randomized clinical trial compared 2 approaches to addressing social risks in a pediatric urgent care setting and found no statistically significant differences in the social risk and child and caregiver health effects of providing written resources at the point of care with vs without in-person longitudinal navigation services. Caregivers in both groups reported fewer social risks and improved child and caregiver health 6 months after the intervention. These findings deepen understanding of effective doses of social risk–related interventions.
Related collections
Most cited references51
- Record: found
- Abstract: found
- Article: not found
The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review.
- Record: found
- Abstract: not found
- Article: not found
Who's Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091
- Record: found
- Abstract: not found
- Article: not found