- Record: found
- Abstract: found
- Article: found
Influence of rebubbling on anterior segment parameters and refractive outcomes in eyes with DMEK for Fuchs endothelial dystrophy
Read this article at
Abstract
Purpose
To evaluate the potential impact of rebubbling on the anterior segment parameters and refractive outcomes in patients with graft detachment following uneventful DMEK for Fuchs endothelial dystrophy (FED).
Methods
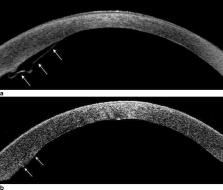
Retrospective institutional cohort study of comparing 34 eyes of 31 patients with rebubbling for graft detachment following Descemet membrane endothelial keratoplasty (DMEK) to 33 eyes of 28 patients with uneventful DMEK. Main outcome parameters were various corneal parameters obtained by Scheimpflug imaging, refractive outcome, corrected distance visual acuity (CDVA), and endothelial cell density (ECD).
Results
Anterior and posterior corneal astigmatism, corneal densitometry, central corneal thickness, and anterior chamber depth and volume showed no significant differences. Preoperative distribution of astigmatism axis orientations showed a high proportion of anterior corneal with-the-rule astigmatism (71%) in eyes requiring rebubbling. Mean postoperative cylinder in the rebubbling group (1.21 ± 0.85 D) was significantly higher compared to the controls ( p = 0.04), while differences in spherical equivalent (SE) were insignificant ( p = 0.24). Postoperative CDVA was 0.11 ± 0.11 in the control group compared to 0.21 ± 0.17 in the rebubbling group ( p = 0.03). Eyes with subsequent rebubbling demonstrated a significantly higher endothelial cell loss (56% versus 37%) ( p < 0.001).
Conclusion
Apart from higher cylinder values, refractive outcome and corneal parameters assessed by Scheimpflug imaging were comparable in eyes with rebubbling and controls. However, a reduced visual acuity and an increased endothelial cell loss should be taken into consideration prior to rebubbling especially in eyes with circumscribed graft detachment.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Descemet membrane endothelial keratoplasty (DMEK).
- Record: found
- Abstract: found
- Article: not found
Normative values for corneal densitometry analysis by Scheimpflug optical assessment.
- Record: found
- Abstract: found
- Article: not found