- Record: found
- Abstract: found
- Article: found
Repair of gastro-tracheobronchial fistula after esophagectomy for esophageal cancer using intercostal muscle and latissimus dorsi muscle flaps: a case report
Read this article at
Abstract
Background
Gastro-tracheobronchial fistula after esophagectomy is a rare but life-threatening complication associated with high mortality. Several authors reported postoperative management of tracheobronchial fistula. However, treatment is demanding and challenging, and the strategy is still controversial.
Case presentation
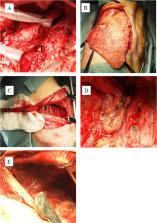
A 64-year-old man underwent thoracoscopic esophagectomy with two-field lymph node dissection and gastric conduit reconstruction by an intrathoracic anastomosis for esophageal cancer at a local hospital in June 2013. After surgery, a gastro-tracheal fistula and a gastro-bronchial fistula of the left main bronchus were diagnosed, and the patient was referred to our hospital for the management of the gastro-tracheobronchial fistula. CT and bronchoscopy and esophagogastroduodenoscopy performed at our hospital revealed that the gastro-bronchial fistula of the left main bronchus was cured by packing with the omentum from the gastric conduit and the gastro-tracheal fistula located 3 cm above the carina remained open. We concluded that the fistula would not resolve without further surgical procedure. However, such an operation was expected to be difficult and to need much time due to severe adhesion among the gastric conduit and/or trachea, bronchus, lung, and chest wall. Therefore, a two-stage operation was planned for safety and outcome certainty. The first operation was performed to close the fistula in October 2013. The gastric conduit was separated from the trachea and resected; then, the fistula was sutured and covered by intercostal muscle and latissimus dorsi muscle flaps. A month after the first operation, reconstruction with pedunculated jejunum was performed via the percutaneous route. The patient’s postoperative course was uneventful.
Conclusion
If the omentum is not observed between the gastric conduit and the tracheobronchus when a gastro-tracheobronchial fistula occurs after esophagectomy, surgeons should perform surgical treatment because conservative treatment is unlikely to cure. During surgery, the use of two types of muscle flaps, such as the intercostal muscle and the latissimus dorsi muscle flaps, is helpful for the closure of gastro-tracheobronchial fistulas.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Ten cases of gastro-tracheobronchial fistula: a serious complication after esophagectomy and reconstruction using posterior mediastinal gastric tube.
- Record: found
- Abstract: found
- Article: not found
Management of Tracheo- or Bronchoesophageal Fistula After Ivor-Lewis Esophagectomy.
- Record: found
- Abstract: found
- Article: not found