- Record: found
- Abstract: found
- Article: found
Risks of cardiovascular diseases associated with dipeptidyl peptidase-4 inhibitors and other antidiabetic drugs in patients with type 2 diabetes: a nation-wide longitudinal study
Read this article at
Abstract
Background
Several antidiabetic drugs (i.e., sulfonylureas; SU, rosiglitazone) have been reported to be associated with increased risks of cardiovascular diseases (CVD) in patients with type 2 diabetes mellitus (T2DM). Dipeptidyl peptidase-4 inhibitors (DPP4i) are newly available antidiabetic drugs. Most studies only compared DPP4i with a placebo or SU, or targeted a specific CVD event of interest (i.e., heart failure; HF). Comparative research of CVD risks of DPP4i with other antidiabetic drugs (i.e., metformin, thiazolidinediones, meglitinides, acarbose, and insulin) remains scarce. This study was aimed to assess comparative risks of CVD, including ischemic stroke, myocardial infarction (MI) and HF, and hypoglycemia of DPP4i with other antidiabetic drugs.
Methods
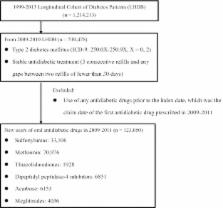
We utilized Taiwan’s National Health Insurance Research Database. A total of 123,050 T2DM patients newly prescribed oral antidiabetic treatments were identified in 2009–2010 and followed until 2013. Outcome endpoints included a composite of CVD events: hospitalizations for ischemic stroke, MI and HF, and hypoglycemia. Time-varying Cox proportional hazards regression was applied to assess the time to event hazards of various antidiabetic drugs, adjusted for patients’ demographics, comorbidity, diabetic complications, and co-medications. Additional analyses were performed for the patients with and without CVD history, respectively.
Results
DPP4i users had significantly lower CVD risks as compared to that of non-DPP4i users (adjusted hazard ratio [aHR]: 0.83, 95 % confidence interval [CI]: 0.76–0.91). Compared to DPP4i users, meglitinides (aHR 1.3, 95 % CI 1.20–1.43) and insulin users (aHR 3.73, 95 % CI 3.35, 4.14) had significantly higher risks for composite CVD, as well as those for stroke, MI, HF, and hypoglycemia. Additionally, metformin users had significantly lower risks for composite CVD risk (aHR 0.87, 95 % CI 0.79–0.94), as well as those for MI, HF, and hypoglycemia, as compared to those of DPP4i users. Although there was a trend toward low CVD risks in pioglitazone users, the role of potential confounding by indication cannot be excluded.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial.

- Record: found
- Abstract: found
- Article: found
Validation of Acute Myocardial Infarction Cases in the National Health Insurance Research Database in Taiwan
- Record: found
- Abstract: found
- Article: not found