- Record: found
- Abstract: found
- Article: found
Arthroscopic Bone Graft Procedure Combined With Arthroscopic Subscapularis Augmentation for Recurrent Anterior Instability With Glenoid Bone Defect
Read this article at
Abstract
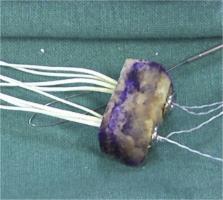
Glenoid bone loss and capsular deficiency represent critical points of arthroscopic Bankart repair failures. The purpose of this Technical Note is to present an all-arthroscopic bone block procedure associated with arthroscopic subscapularis augmentation for treating glenohumeral instability with glenoid bone loss and anterior capsulolabral deficiency. Two glenoid tunnels are set up from the posterior to the anterior side using a dedicated bone block guide, and 4 buttons are used to fix the graft to the glenoid. The subscapularis tenodesis is performed using a suture tape anchor. This combined arthroscopic technique (bone block associated with arthroscopic subscapularis augmentation) could be a valid and safe alternative to the arthroscopic or open Latarjet procedures.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
The Bankart procedure: a long-term end-result study.
- Record: found
- Abstract: not found
- Article: not found
[Treatment of recurrent dislocation of the shoulder].
- Record: found
- Abstract: found
- Article: not found