- Record: found
- Abstract: found
- Article: found
Five year risk assessment and treatment patterns in patients with chronic thromboembolic pulmonary hypertension
Read this article at
Abstract
Aims
Repeated risk assessments and treatment patterns over long time are sparsely studied in chronic thromboembolic pulmonary hypertension (CTEPH); thus, we aimed to investigate changes in risk status and treatment patterns in incident patients with CTEPH over a 5 year period.
Methods and results
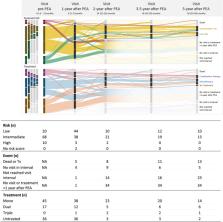
Descriptive and explorative study including 311 patients diagnosed with CTEPH 2008–2019 from the Swedish pulmonary hypertension registry, stratified by pulmonary endarterectomy surgery (PEA). Risk and PH‐specific treatment were assessed in surgically treated (PEA) and medically treated (non‐PEA) patients at diagnosis and up to 5 years follow‐up. Data are presented as median (Q1–Q3), count or per cent. Prior to surgery, 63% in the PEA‐group [ n = 98, age 64 (51–71) years, 37% female] used PH‐specific treatment and 20, 69, and 10% were assessed as low, intermediate or high risk, respectively. After 1 year post‐surgery, 34% had no PH‐specific treatment or follow‐up visit registered despite being alive at 5 years. Of patients with a 5 year visit ( n = 23), 46% were at low and 54% at intermediate risk, while 91% used PH‐specific treatment.
In the non‐PEA group [ n = 213, age 72 (65–77) years, 56% female], 28% were assessed as low, 61% as intermediate and 11% as high risk. All patients at high risk versus 50% at low risk used PH‐specific treatment. The 1 year mortality was 6%, while the risk was unchanged in 57% of the patients; 14% improved from intermediate to low risk, and 1% from high to low risk. At 5 years, 27% had a registered visit and 28% had died. Of patients with a 5 year visit ( n = 58), 38% were at low, 59% at intermediate and 1% at high risk, and 86% used PH‐specific treatment.
Conclusions
Risk status assessed pre‐surgery did not foresee long‐term post‐PEA risk and pre‐surgery PH‐specific treatment did not foresee long‐term post‐PEA treatment. Medically treated CTEPH patients tend to remain at the same risk over time, suggesting a need for improved treatment strategies in this group.
Related collections
Most cited references23
- Record: found
- Abstract: not found
- Article: not found
2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT).

- Record: found
- Abstract: found
- Article: found
Chronic thromboembolic pulmonary hypertension
- Record: found
- Abstract: found
- Article: not found