- Record: found
- Abstract: found
- Article: found
Randomized comparison of oblique and perpendicular stabilizers for minimally invasive repair of pectus excavatum

Read this article at
Abstract
OBJECTIVES
Bar dislocation is one of the most feared complications of the minimally invasive repair of pectus excavatum.
METHODS
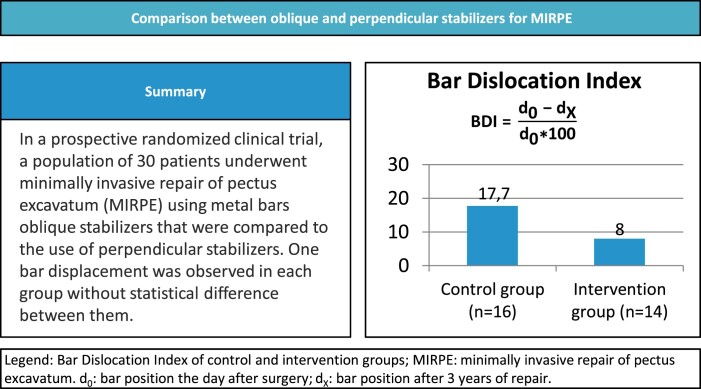
Prospective randomized parallel-group clinical trial intending to assess whether oblique stabilizers can reduce bar displacement in comparison with regular stabilizers used in minimally invasive repair of pectus excavatum. Additionally, we evaluated pain, quality of life and other postoperative complications. Participants were randomly assigned to surgery with perpendicular ( n = 16) or oblique stabilizers ( n = 14) between October 2017 and September 2018 and followed for 3 years. Bar displacements were evaluated with the bar displacement index. Pain scores were evaluated through visual analogue scale and quality of life through the Pectus Excavatum Evaluation Questionnaire.
RESULTS
Control group average displacement index was 17.7 (±26.7) and intervention group average displacement index was 8.2 (±10.9). There was 1 reoperation in each group that required correction with 2 bars. Bar displacement was similar among groups ( P = 0.12). No other complications were recorded. There was no statistically significant difference on pain score. There was a significant difference between pre- and postoperative composite scores of the participants’ body image domain and psycho-social aspects in both groups. The difference between the pre- and postoperative participants’ perception of physical difficulties was greater and statistically significant in the intervention group.
Abstract
Pectus excavatum (PE) is associated with shortness of breath, exercise intolerance, low self-esteem and depression [1–3] and to date there is no effective non-invasive treatment [4].
Related collections
Most cited references29

- Record: found
- Abstract: found
- Article: not found
CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials
- Record: found
- Abstract: found
- Article: not found
Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients.
- Record: found
- Abstract: found
- Article: not found